
To analyze whether admission on weekends or public holidays (WHA) influences the management (performance of angioplasty, percutaneous coronary intervention [PCI]) and outcomes (in-hospital mortality) of patients hospitalized for acute coronary syndrome in the Spanish National Health System compared with admission on weekdays.
MethodsRetrospective observational study of patients admitted for ST-segment elevation myocardial infarction (STEMI) or for non–ST-segment elevation acute coronary syndrome (NSTEACS) in hospitals of the Spanish National Health system from 2003 to 2018.
ResultsA total of 438 987 episodes of STEMI and 486 565 of NSTEACS were selected, of which 28.8% and 26.1% were WHA, respectively. Risk-adjusted models showed that WHA was a risk factor for in-hospital mortality in STEMI (OR, 1.05; 95%CI,1.03-1.08; P < .001) and in NSTEACS (OR, 1.08; 95%CI, 1.05-1.12; P < .001). The rate of PCI performance in STEMI was more than 2 percentage points higher in patients admitted on weekdays from 2003 to 2011 and was similar or even lower from 2012 to 2018, with no significant changes in NSTEACS. WHA was a statistically significant risk factor for both STEMI and NSTEACS.
ConclusionsWHA can increase the risk of in-hospital death by 5% (STEMI) and 8% (NSTEACS). The persistence of the risk of higher in-hospital mortality, after adjustment for the performance of PCI and other explanatory variables, probably indicates deficiencies in management during the weekend compared with weekdays.
Keywords
In 2001, a study indicated that patients admitted during the weekend had higher mortality than those admitted on weekdays.1 Since then, numerous studies have analyzed the “weekend effect” in a large variety of populations of patients, diseases, health care providers, and health care systems.2
Identification of the weekend effect led to the implementation of major health care policy interventions (eg, the 7-day hospital services program in the UK3,4), which have caused considerable controversy, such as the first large-scale physician strike in the National Health Service in 40 years.5
The debate surrounding the existence and causes of the weekend effect continues. While some researchers have questioned its existence,6 others have highlighted the ongoing uncertainty regarding its causes.7
The existence of the weekend effect has also been examined in the Spanish National Health System (SNHS) in terms of different aspects of health care quality, including mortality,8–14 but, as far as we know, no studies have explored its relationship with acute coronary syndrome (ACS) in Spain.
Therefore, the objective of our study was to analyze if weekend or public holiday admission (WHA), vs weekday admission, affects the management (performance of angioplasty and primary percutaneous coronary intervention [PCI]) and outcomes (in-hospital mortality) of patients hospitalized for ACS in the SNHS.
METHODSPopulationA retrospective observational study was performed in patients admitted for ACS in SNHS hospitals between January 1, 2003, and December 31, 2018. The data source was the Minimum Data Set (MDS) of the SNHS, which includes data on the demographic characteristics of hospitalized patients, as well as administrative variables regarding the care process and clinical variables related to diagnoses and procedures, coded using the International Classification of Diseases (ICD) 9th (2003-2005) and 10th (2016-2018) editions.15 The ACS population was divided into 2 groups: ST-segment elevation acute myocardial infarction (STEMI) and non–ST-segment elevation acute coronary syndrome (NSTEACS) (non–ST-segment elevation acute myocardial infarction and unstable angina). The ICD-9 and -10 (Clinical Modification) codes used to identify diagnoses and procedures are detailed in . PCI performance and in-hospital mortality were compared between WHA patients (considering national holidays alone) and those admitted on weekdays (from Monday to Friday, except national holidays).
To improve data consistency, transfers between hospitals were consolidated in a single episode that was attributed to the more complex hospital if the destination hospital was identified. In addition, episodes corresponding to patients younger than 18 years were excluded, as well as those corresponding to patients who were discharged to home and had hospital stays of 1 day or less and to patients registered as voluntary discharges with an unknown discharge location or with discharges to another hospital that could not be resolved after concatenation.
Statistical analysisQuantitative variables are presented as mean ± standard deviation and categorical variables as frequency and percentage.
For adjustment by the risk of in-hospital mortality, models were based on the methodology of the Centers for Medicare and Medicaid Services. The independent variables were those included in the 30-day acute myocardial infarction mortality model,16 with adaptation of the Centers for Medicare and Medicaid Services model to the structure of the MDS data. The secondary diagnoses were then grouped according to the clinical condition categories developed by Pope et al.17 and updated annually by the Agency for Healthcare Research and Quality.16
To analyze the impact of the type of hospital on the association between WHA or weekday admission and in-hospital mortality, hospitals were classified by the availability of cardiology-related resources using RECALCAR criteria.18 To differentiate the impact of weekend admission from national holiday admission, the independent variable WHA was separated into 2 components: a) national holiday admission (dichotomous); and b) weekday of hospital admission (categorical, with Tuesday as reference, to clarify the impact of Friday and Monday, the days immediately before and after the weekend).
In-hospital mortality was adjusted using multilevel logistic regression models.19 All adjustment models specifically considered comorbidities with statistical significance and an odds ratio (OR) < 1.0. The adjustment models were estimated using backward elimination; the significance thresholds for the selection and elimination of factors were P < .05 and P ≥ .10, respectively. Using the specified models, we calculated risk-adjusted in-hospital mortality rates (RAMRs).20 Calibration was analyzed graphically after patients were grouped in deciles with regard to predicted probabilities, and predicted vs observed mean probabilities were tabulated, as well as discrimination using the area under the receiver operating characteristic (ROC) curve.
Quantitative variables were compared using the t test for 2 categories. Categorical variables were compared using the chi-square test or Fisher exact test.
Temporal trends in mortality and PCI performance during the study period were assessed using a Poisson regression model with year as the sole independent variable. In all models, we calculated the incidence rate ratios (IRRs) and their 95% confidence intervals (95%CIs).
As sensitivity analysis, we evaluated the changes over time in the frequency of PCI performance considering, in both groups (STEMI and NSTEACS), the impact of WHA vs weekday admission; 2 periods were defined, taking as cutoff the year in which a significant change was detected, for which the multilevel model was adjusted by including PCI performance among the independent variables.
All comparisons were 2-sided and differences were considered significant at P < .05. Statistical analyses were performed with STATA 16 and SPSS v21.0.
RESULTSIn-hospital mortalityIn total, 475 362 STEMI episodes and 548 176 NSTEACS episodes were identified from 2003 to 2008; after exclusions (), we obtained a study population of 438 987 (92.3%) and 486 565 (88.8%) episodes, respectively. Of these, 126 528 (28.8%) and 127 188 (26.1%) were WHAs, without significant variations in these proportions during the study period. The profiles of the patients admitted on weekdays and on weekends or public holidays were notably homogeneous in the 2 groups (table 1 and table 2), with the exception of a slightly higher rate of cardiogenic shock and cardiorespiratory failure in patients with NSTEACS admitted at the weekend.
Differences in the profile of patients admitted for STEMI on weekdays or public holidays
| Weekday (n = 312 459) | Holiday (n = 126 528) | Difference | P | |
|---|---|---|---|---|
| Age, y | 67.3 ± 14.2 | 66.6 ± 14.4 | −1% | < .001 |
| Female sex, % | 29.0 | 28.0 | −4% | < .001 |
| Anterior wall AMI | 36.2 | 36.7 | 2% | < .001 |
| AMI in regions other than anterior wall | 51.9 | 52.0 | 0% | .258 |
| History of CABG | 1.3 | 1.2 | −7% | .010 |
| History of PCI | 8.1 | 8.3 | 2% | .043 |
| Metastatic cancer, leukemia, other severe cancers (CC 8–9) | 1.0 | 0.9 | −6% | .059 |
| DM or DM complications except proliferative retinopathy (CC 17–19, 123) | 28.7 | 27.8 | −3% | < .001 |
| Chronic liver disease (CC 27–29) | 1.0 | 1.0 | −1% | .707 |
| Dementia or other specific brain disorders (CC 51–53) | 3.4 | 3.3 | −3% | .053 |
| Major psychiatric disorders (CC 57–59) | 0.7 | 0.7 | −6% | .106 |
| Hemiplegia, paraplegia, paralysis, functional disability (CC 70–74, 103–104, 189–190) | 1.8 | 1.8 | −2% | .425 |
| Cardiogenic shock (R57.0) | 5.5 | 5.7 | 5% | .001 |
| Cardiorespiratory failure and shock (CC 84), except cardiogenic (R57.0) | 6.8 | 6.9 | 1% | .237 |
| Heart failure (CC 85) | 19.8 | 19.5 | −2% | .007 |
| AMI complications (tendinous cord or papillary muscle rupture)* | 0.1 | 0.1 | 0% | .942 |
| Other AMI complications* | 0.3 | 0.3 | 0% | .939 |
| Rheumatic heart disease or valve disease (CC 91) | 12.5 | 12.1 | −4% | .000 |
| Hypertension (CC 95) | 46.7 | 46.1 | −1% | .000 |
| Stroke (CC 99–100) | 1.0 | 1.0 | −1% | .801 |
| Cerebrovascular disease (CC 101–102, 105) | 2.3 | 2.1 | −7% | .002 |
| Vascular disease and complications (CC 106–108) | 5.9 | 5.8 | −2% | .189 |
| Chronic obstructive pulmonary disease (CC 111) | 7.9 | 7.7 | −2% | .031 |
| Pneumonia (CC 114–116) | 2.1 | 2.1 | 1% | .792 |
| Kidney failure (CC 135–140) | 10.4 | 9.9 | −4% | < .001 |
AMI, acute myocardial infarction; CABG, coronary artery bypass surgery; CC, Condition Categories (Pope et al.17); DM, diabetes mellitus; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation acute myocardial infarction.
Values represent percentage or mean ± standard deviation.
Differences in the profile of patients admitted for NSTEACS on weekdays or public holidays
| Weekday (n = 359 377) | Holidayn = 12 188 | Difference | P | |
|---|---|---|---|---|
| Age, y | 71.3 ± 12.7 | 71.4 ± 12.9 | 0% | < .001 |
| Female sex | 35.6 | 35.6 | 0% | .484 |
| Anterior wall AMI | 0.2 | 0.2 | 11% | .091 |
| History of CABG | 4.9 | 4.9 | 0% | .841 |
| History of PCI | 15.3 | 15.0 | −2% | .003 |
| Metastatic cancer, leukemia, other severe cancers (CC 8–9) | 1.2 | 1.3 | 6% | .060 |
| DM or DM complications except proliferative retinopathy (CC 17–19, 123) | 37.2 | 37.7 | 1% | .001 |
| Chronic liver disease (CC 27–29) | 1.2 | 1.2 | −1% | .889 |
| Dementia or other specific brain disorders (CC 51–53) | 3.4 | 3.6 | 7% | < .001 |
| Major psychiatric disorders (CC 57–59) | 0.5 | 0.5 | 0% | .929 |
| Hemiplegia, paraplegia, paralysis, functional disability (CC 70–74, 103–104, 189–190) | 2.2 | 2.3 | 4% | .095 |
| Cardiogenic shock (R57.0) | 1.3 | 1.5 | 11% | < .001 |
| Cardiorespiratory failure and shock (CC 84), except cardiogenic (R57.0) | 5.0 | 5.6 | 11% | < .001 |
| Heart failure (CC 85) | 20.7 | 21.7 | 5% | < .001 |
| AMI complications (tendinous cord or papillary muscle rupture)* | 0.0 | 0.0 | 0% | .775 |
| Other AMI complications* | 0.1 | 0.1 | 0% | .769 |
| Rheumatic heart disease or valve disease (CC 91) | 15.8 | 16.1 | 2% | .047 |
| Hypertension (CC 95) | 52.9 | 52.6 | −1% | .038 |
| Stroke (CC 99–100) | 0.5 | 0.5 | −4% | .305 |
| Cerebrovascular disease (CC 101–102, 105) | 3.3 | 3.4 | 4% | .021 |
| Vascular disease and complications (CC 106–108) | 9.0 | 9.0 | 0% | .857 |
| Chronic obstructive pulmonary disease (CC 111) | 10.3 | 10.4 | 1% | .177 |
| Pneumonia (CC 114–116) | 1.7 | 1.8 | 8% | .001 |
| Kidney failure (CC 135–140) | 14.7 | 15.2 | 4% | < .001 |
AMI, acute myocardial infarction; CABG, coronary artery bypass surgery; CC, Condition Category (Pope et al.17); DM, diabetes mellitus; NSTEACS, non–ST-segment elevation acute coronary syndrome; PCI, percutaneous coronary intervention.
Values represent percentage or mean ± standard deviation.
The crude mortality rate during the study period was 11.7% in the STEMI group and 5.5% in the NSTEACS group. Both groups exhibited slightly but significantly higher mortality between weekday admission and WHA (STEMI, 11.6% vs 11.9%, P = .008; NSTEACS, 5.3% vs 5.9%, P < .001). In STEMI, the crude mortality rate significantly fell during the study period (IRR = 0.998; 95%CI, 0.998-0.999; P < .001) in both patients admitted on weekdays (IRR = 0.999; 95%CI, 0.999-0.999; P < .001) and those admitted on public holidays (IRR = 0.998; 95%CI, 0.998-0.999; P < .001). In contrast, in the NSTEACS group, the crude mortality rate increased during the study period (IRR = 1.004; 95%CI, 1.000-1.010; P = .002) in both patients admitted on weekdays (IRR = 1.003; 95%CI, 1.000-1.010; P = .049) and those admitted on public holidays (IRR = 1.004; 95%CI, 1.002-1.007; P = .003).
The adjusted in-hospital mortality risk models for both STEMI and NSTEACS showed very good discrimination (ROC, 0.88 and 0.87, respectively) and calibration (, , , and ). Both groups exhibited a significant trend for a decrease in the RAMR for both weekday admissions and WHAs (total RAMR of each group, IRR = 0.999; 95%CI, 0.999-0.999; and IRR = 0.996; 95%CI, 0.995-0.997; both P < .001). The WHA variable was found to be a risk factor in risk-adjusted models for STEMI (OR = 1.05; 95%CI, 1.03-1.08; P < .001) and NSTEACS (OR = 1.08; 95%CI, 1.05-1.12; P < .001).
When we analyzed the day of admission and admission on national holidays separately instead of together in WHA ( and ), there was a greater effect in both STEMI and NSTEACS of national holiday admission (OR = 1.11; 95%CI, 1.03-1.19; P < .001; and OR = 1.15; 95%CI, 1.05-1.26; P < .001) than admission on Saturday or Sunday (STEMI: OR = 1.04; 95%CI, 1.00-1.09; P = .04; and OR = 1.03; 95%CI, 0.99-1.08; P = .13; NSTEACS: OR = 1.08; 95%CI, 1.03-1.14; P < .001; and OR = 1.08; 95%CI, 1.02-1.14; P = .01).
In STEMI, hospitals with a catheterization laboratory were protective factors (RECALCAR types 3, 4, and 5, OR = 0.86, OR = 0.80, and OR = 0.64, respectively; P < .001); the same effect was found in NSTEACS, although the results were only significant for type 5 hospitals (with catheterization laboratories but without beds specifically assigned to cardiology) (type 3, OR = 0.95; type 4, OR = 0.93 [P > .05]; type 5, OR = 0.72; P < .001); in both cases, WHA remained a risk factor (STEMI: OR = 1.05; NSTEACS: OR = 1.08; P < .001).
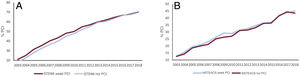
Percutaneous coronary interventionFrom 2003 to 2018, the PCI performance rate was significantly lower in patients with WHA than in those admitted on weekdays in both STEMI (46.8% vs 48.7%; P < .001) and NSTEACS (28.2% vs 29.1%; P < .001). However, the differences seemed to have no clinical relevance. In contrast, the rate was significantly increased in STEMI in both patients admitted on weekdays (IRR = 1.069; 95%CI, 1.055-1.082, P < .001) and WHA patients (IRR = 1.078; 95%CI, 1.063-1.092; P < .001), and the same tendency was found in NSTEACS (weekday admission, IRR = 1.072; 95%CI, 1.061-1.083; P < .001; WHA, IRR = 1.077; 95%CI, 1.066-1.087; P < .001) (figure 1).
Sensitivity analysis: weekend/holiday effect and percutaneous coronary interventionThrough analysis of the changes over time in the frequency of PCI performance, a significant change was observed in 2012 in both groups (STEMI and NSTEACS) in patients admitted on weekdays or weekends/public holidays, and 2 study subperiods were identified: 2003 to 2011 and 2012 to 2018. The rate of PCI performance in STEMI was more than 2 percentage points higher in patients admitted on weekdays from 2003 to 2011 and similar or even lower from 2012 to 2018 (figure 1), with a significant interaction between the year and a lower difference in the rate of PCI performance (the later the period, the lower the difference) (P = .006). In contrast, this interaction was not found between the year and the difference in PCI performance in NSTEACS (P = .253).
The performance of PCI in STEMI had a protective effect against in-hospital mortality at all admission times and in both periods (2003-2011, OR = 0.25; 95%CI, 0.24-0.26; P < .001; 2012-2018, OR = 0.29; 95%CI, 0.27-0.30; P < .001). The same effect was observed in NSTEACS (2003-2011, OR = 0.36; 95%CI, 0.33-0.39; P < .001; 2012-2018, OR = 0.34; 95%CI, 0.32-0.37; P < .001).
The effect of WHA was identified as a significant risk factor in both periods in both STEMI and NSTEACS, even when PCI performance was considered in the multilevel adjustment models for in-hospital mortality (table 3).
Effect of weekend admission on in-hospital mortality in STEMI and NSTEACS
| 2003-2018 | 2003-2011 | 2012-2018 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | P | 95%CI | OR | P | 95%CI | OR | P | 95%CI | ||||
| STEMIa | ||||||||||||
| Weekend | 1.05 | < .001 | 1.03 | 1.08 | 1.05 | .004 | 1.02 | 1.08 | 1.06 | .010 | 1.01 | 1.10 |
| Weekend + PCI | 1.03 | .048 | 1.00 | 1.05 | 1.03 | .047 | 1.00 | 1.07 | 1.05 | .037 | 1.01 | 1.09 |
| NSTEACSb | ||||||||||||
| Weekend | 1.08 | < .001 | 1.05 | 1.11 | 1.08 | < .001 | 1.03 | 1.12 | 1.08 | .002 | 1.03 | 1.13 |
| Weekend + PCI | 1.07 | < .001 | 1.04 | 1.11 | 1.07 | .001 | 1.03 | 1.12 | 1.07 | .007 | 1.02 | 1.12 |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; CABG, coronary artery bypass surgery; NSTEACS, non–ST-segment elevation acute coronary syndrome; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation acute myocardial infarction.
Adjusted by age, sex, history of CABG, cancer, diabetes mellitus, chronic kidney disease, dementia, severe mental illness, hemiplegia, paraplegia, functional disability, cardiogenic shock, cardiorespiratory disorder other than cardiogenic shock, heart failure, AMI complications, unstable angina, stroke, cerebrovascular disease, vascular disease, pneumonia, and kidney failure.
Adjusted by age, sex, anterior wall AMI, cancer, chronic kidney disease, dementia, severe mental illness, hemiplegia, paraplegia, functional disability, cardiogenic shock, cardiorespiratory disorder other than cardiogenic shock, heart failure, AMI complications, unstable angina, stroke, cerebrovascular disease, vascular disease, pneumonia, kidney failure, and trauma and other lesions.
Our results show than WHA in SNHS hospitals increases the risk of in-hospital death by 5% in STEMI patients and 8% in NSTEACS patients. These findings are in line with those reported in the literature, although the underlying cause is still unclear.
In the United States, higher mortality has been reported in patients admitted during the weekend for ACS,21 as well as for non–ST-segment elevation acute myocardial infarction.22 In both studies, the elevated mortality was related to fewer interventional procedures in these patients during the weekend. However, no differences were found in mortality in more recent periods (2006-2016).23 A meta-analysis including 18 European countries and those from other continents concluded that the weekend effect was associated with a slight increase (6%) in short-term ACS mortality.24 That meta-analysis found no significant differences after the analysis was restricted to studies performed from 2005 onwards, although the magnitude of the difference in mortality was maintained.
The widespread implementation of the Infarction Code Program25 probably explains the first reduction and the practical erasure of the difference in 2017 and 2018 in the primary PCI percentage between weekdays and weekends in STEMI. However, the persistent difference in mortality may indicate the involvement of other elements of the health care process,26 as well as the performance of PCI. These elements include delays during weekends and public holidays vs weekdays in patient contact with the emergency health care system and in the referral of patients from the emergency services of primary care centers and hospitals that are not Infarction Code Program referral centers, in addition to lower agility in the activation of the catheterization team performing the primary PCI or in the functioning of the receiving center itself. Light could be shed on this matter using the time comparison information for weekdays vs weekends/public holidays in the health system available in the Infarction Code Program registry.
In this study, the effect of WHA on in-hospital mortality was slightly higher in NSTEACS than in STEMI. The apparently contradictory finding of increased crude in-hospital mortality in NSTEACS during the study period, in contrast to the reduced adjusted mortality, is probably explained by the shifting of age at presentation and, thus, of comorbidities, which highlights the need for risk adjustments of trend analysis.27 The greater effect of WHA on NSTEACS is in line with other studies reporting a greater delay in the performance of early coronary angiography during the weekend,28–31 an approach recommended by clinical practice guidelines for high- or very high-risk patients,32 even though these studies are contradictory regarding higher mortality at the weekend. As in STEMI, the risk stratification of in-hospital death by PCI performance showed higher risk-adjusted mortality in NSTEACS for WHA. In principle, this could lead to analysis of the same causes associated with the value chain of the health care process as those described for STEMI, although it must be remembered that the differences in the PCI performance rates between WHA and weekday admissions are small and might not be clinically significant. The MDS does not provide information on the timing of PCI performance. Thus, in contrast to STEMI, in which practically all PCIs without concomitant fibrinolysis in the episode are primary PCIs, we cannot rule out the possibility that, in NSTEACS, PCIs were delayed vs the guideline recommendations.
The higher in-hospital mortality in both STEMI and NSTEACS during the weekend/public holidays could be due to the patient profile, because these patients could be more severe than those admitted during the week. However, risk-adjusted mortalities were compared in this study and no significant epidemiological differences (eg, age, sex, and comorbidities) were found in the profile of patients admitted at the weekend or on weekdays (table 1 and table 2), and the percentages of cardiogenic shock, cardiorespiratory failure, and heart failure were practically the same in the 2 groups. The meta-analysis by Kwok et al.24 also failed to find differences in the profile of patients that would explain the higher mortality on the weekend, with the most plausible explanations being staff and organizational differences between weekdays and weekends. In addition, some studies indicate that a lack of information at handovers during WHA can aggravate the clinical situation of patients and that the use of checklists or standardized handover models could mitigate these effects.33,34
LimitationsOur study has several limitations. Due to its observational and retrospective design, we cannot exclude the possible existence of a selection bias and a possible effect of unmeasured confounding factors. In addition, given the data source, there may be biases because the MDS does not collect information on certain clinically relevant variables—such as date and time of PCI performance, the artery affected, multivessel disease, and left ventricular ejection fraction—and the quality of the data on diagnoses and procedures performed in patients during their hospitalization depends on the coding adequacy in each hospital. Moreover, the MDS does not provide information allowing a comparison of outcomes between WHA patients and outcomes obtained on weekdays by the timing of catheterization alert activation. However, in contrast, one of the strengths is that the use of administrative databases for investigating health outcomes has been validated through their comparison with data extracted from medical records,35 as well as that the MDS provides considerable statistical power because it includes a nationwide population over a large time period and with established validity for the study of ACS in the SNHS.36
In contrast to the models developed by the Centers for Medicare & Medicaid Services, the MDS did not record comorbidities present at admission until 2016, which is why the secondary diagnoses used as adjustment variables could be comorbidities or complications that occasionally reflect inadequate management.34 Nonetheless, the models used in this study are comparable with other published models regarding their discrimination capacity.16 In addition, it must be remembered that the adjustment models include confounding factors that are impossible to consider and may have a significant impact.
CONCLUSIONSIn patients with ACS, WHA in SNHS hospitals increases the risk of in-hospital death by 5% in STEMI patients and 8% in NSTEACS patients. Although the higher risk in STEMI could be due to a lower rate of PCI in WHAs, the risk increase was maintained from 2012 to 2018, a period in which the PCI rate was the same on weekdays and weekends, probably due to the widespread implementation of the Infarction Code Program. Analysis of the differences in care times between weekdays and weekends/public holidays in health care services with registries (in the absence of a national registry) could shed light on which part of the observed effect may be due to this cause and which is due to management deficiencies during the weekend vs weekdays that could reflect the general functioning of hospitals, as well as the entire value chain of the health care process.
FUNDINGThis work has been funded by an unconditional grant from the Fundación Interhospitalaria de Investigación Cardiovascular (FIC) FIC/01/21 to the Fundación Instituto para la Mejora de la Asistencia Sanitaria.
AUTHORS’ CONTRIBUTIONSA. Fernández-Ortiz: conception, design, and critical revision of the manuscript. M.C. Bas Villalobos: conception, design, and critical revision of the manuscript. M. García-Márquez: data acquisition and analysis. J.L. Bernal Sobrino: conception, design, and drafting of the manuscript. C. Fernández-Pérez: data acquisition and analysis. N. del Prado González: data acquisition and analysis. A. Viana Tejedor: critical revision of the manuscript. I. Núñez-Gil: critical revision of the manuscript. C. Macaya Miguel: critical revision of the manuscript. F. Javier Elola Somoza: conception, design, and drafting of the manuscript.
CONFLICTS OF INTERESTNone.
- –
Increased in-hospital mortality has been reported in patients admitted at weekends.
- –
Studies of the “weekend effect” in patients admitted for acute coronary syndrome in different countries are contradictory but generally indicate slightly higher mortality.
- –
Spanish hospitals have shown higher in-hospital mortality associated with the weekend.
- –
This is the first study to analyze the weekend effect regarding the management of acute coronary syndrome in Spain.
- –
Our results indicated higher mortality in patients admitted for acute coronary syndrome during weekends and on public holidays, even in ST-segment elevation acute myocardial infarction and despite the widespread implementation of the Infarction Code Program and the erasure of differences in the primary angioplasty percentage between patients admitted on weekdays or public holidays.
We thank the Spanish Ministry of Health and the Instituto de Información Sanitaria (Institute for Health Information) in particular for granting partial access to the MDS data.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.10.022

![Changes over time in the rate of percutaneous coronary intervention (PCI) performance. A: in ST-segment elevation acute myocardial infarction (STEMI). B: in non–ST-segment acute coronary syndrome (NSTEACS) (weekdays [week] and public holidays [hol]). Changes over time in the rate of percutaneous coronary intervention (PCI) performance. A: in ST-segment elevation acute myocardial infarction (STEMI). B: in non–ST-segment acute coronary syndrome (NSTEACS) (weekdays [week] and public holidays [hol]).](https://static.elsevier.es/multimedia/18855857/0000007500000009/v1_202208220508/S1885585721003753/v1_202208220508/en/main.assets/thumbnail/gr1.jpeg?xkr=eyJpdiI6IlRLNE5lcldvd244Y0hvR2wwM1hYRlE9PSIsInZhbHVlIjoiSkFJWHovMjBaS1JsR01TeU4vTlkyOHltVE1uSXpvQlBvcUcvVEI0TzIvST0iLCJtYWMiOiJmNThiZDhjZTNkMTJhZjAxNjg1Yjk3NjEwOGM1Y2FmNzFlNmMxN2VhODAzODM4ZjY4Y2QzOWI2NDk3YjBiMjhiIiwidGFnIjoiIn0=)