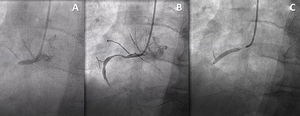
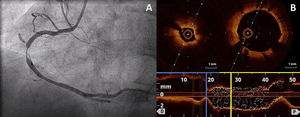
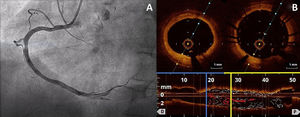
A 60-year-old male smoker was treated by the medical emergency response service for a 4-hour history of oppressive chest pain; the electrocardiogram showed ST-segment elevation in the inferior leads. The patient was transferred to the catheterization laboratory for emergent coronary angiography, which showed acute thrombotic occlusion of the proximal segment of the right coronary artery (figure 1). After successful percutaneous angioplasty of the occlusion and placement of a sirolimus-eluting stent (figure 1B,C), a new focal stenosis was observed adjacent to the distal end of the lesion (figure 2A). The stenosis was reversed by intracoronary nitroglycerin injection. Optical coherence tomography (OCT) showed nonobstructive atherosclerosis at the distal landing zone of the stent graft; no complications were observed and coronary artery spasm was identified as the most likely cause. Stent optimization was performed using the OCT measurements (figure 2B), but the spasm reappeared at the edge of the stent. Again, this was reversed with an intracoronary injection of nitroglycerin (figure 3A). A second OCT scan, however, showed stent malapposition secondary to the increase in vessel caliber (figure 3B,C). The most distal portion of the stent was postdilated again and the patient discharged 4 days later. Vasospasm might be responsible for acquired malapposition following acute coronary syndrome. Informed consent was obtained from the patient for publication of case details.
FundingThis study did not require any funding.
Authors’ ContributionsA. Jerónimo: drafting of manuscript and creation of figures. I.J. Núñez-Gil: creation of figures and review of manuscript drafts. A.I. Fernández-Ortiz: creation of figures and review of manuscript drafts.
Conflicts of InterestNone.