Up to 45% of patients with severe aortic stenosis (AS) have concomitant moderate or severe mitral regurgitation (MR).1 The high rate of multivalvular disease is due to the elevated filling pressures of the left ventricle resulting from the increased afterload due to severe AS and the parallel deterioration of both valves due to the aging process. Clinical practice guidelines recommend surgical repair or replacement of both valves in this scenario, although this recommendation remains controversial due to the limited evidence and the higher mortality associated with this strategy.2 Indeed, many patients undergo single surgical or percutaneous aortic valve replacement. The growing use of transcatheter aortic valve implantation (TAVI) in these patients suggests an improvement in the degree of MR in more than 50% of cases, with a parallel decrease in the cardiac mortality rate during follow-up.3 Therefore, it is crucial to identify patients who could potentially improve in the concomitant degree of MR following TAVI. Previous studies have identified some predictors of MR persistence in this scenario, including calcification of the mitral apparatus, organic valvular disease, mitral annular dilatation, atrial fibrillation, left bundle branch block, and pulmonary hypertension.2 Recently Cortés et al. have determined the impact of these and other factors in 177 patients with moderate or severe MR who underwent TAVI and whose echocardiographic and computed tomography images were centrally analyzed.3 Following characterization of the main predictors of MR persistence, software named the Multivalvular Score was developed. This software is easy to use and helpful to the Heart Team when making clinical decisions about candidates for valve interventions (Figure 1A). This tool is available as open-access software for computers through a link,4 as a free app for smartphones, or as an analog numeric scale, as shown in Figure 1C. The calibration value was 3.960 (P=.776) and discrimination was 0.781 (95%CI, 0.671-0.892).
A: interface of the “Multivalvular Score”. B: ROC curves showing sensitivity and specificity for the initial sample4 and for the validation sample. C: score assigned to each variable and range of scores associated with different likelihoods of mitral regurgitation persistence; the ROC curves below demonstrate an exceptional correlation of the logistic regression and the score system. 95%CI, 95% confidence interval; AUC, area under curve; LBBB, left bundle branch block; MR, mitral regurgitation; ROC, receiver operating characteristic; SE, standard error; SPPA, systolic pressure of pulmonary artery; TAVI, transcatheter aortic valve implantation.
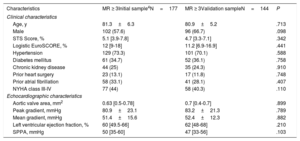
By using this software, we aimed to perform a prospective validation of the score. A total of 144 patients with moderate or severe MR from 4 institutions who underwent TAVI between April, 2009 and June, 2016 were evaluated with the Multivalvular Score and clinical results 1 year after the procedure were compared with the predicted outcomes. The main clinical and imaging characteristics were similar to those of the original study3 and are summarized in Table 1.
Comparison of the Main Clinical and Echocardiographic Characteristics of the Initial and the Validation Samples
| Characteristics | MR ≥ 3Initial sample4N=177 | MR ≥ 3Validation sampleN=144 | P |
|---|---|---|---|
| Clinical characteristics | |||
| Age, y | 81.3±6.3 | 80.9±5.2 | .713 |
| Male | 102 (57.6) | 96 (66.7) | .098 |
| STS Score, % | 5.1 [3.9-7.8] | 4.7 [3.3-7.1] | .342 |
| Logistic EuroSCORE, % | 12 [9-18] | 11.2 [6.9-16.9] | .441 |
| Hypertension | 129 (73.3) | 101 (70.1) | .588 |
| Diabetes mellitus | 61 (34.7) | 52 (36.1) | .758 |
| Chronic kidney disease | 44 (25) | 35 (24.3) | .910 |
| Prior heart surgery | 23 (13.1) | 17 (11.8) | .748 |
| Prior atrial fibrillation | 58 (33.1) | 41 (28.1) | .407 |
| NYHA class III-IV | 77 (44) | 58 (40.3) | .110 |
| Echocardiographic characteristics | |||
| Aortic valve area, mm2 | 0.63 [0.5-0.78] | 0.7 [0.4-0.7] | .899 |
| Peak gradient, mmHg | 80.9±23.1 | 83.2±21.3 | .789 |
| Mean gradient, mmHg | 51.4±15.6 | 52.4±12.3 | .882 |
| Left ventricular ejection fraction, % | 60 [49.5-66] | 62 [48-68] | .210 |
| SPPA, mmHg | 50 [35-60] | 47 [33-56] | .103 |
Values are expressed as No. (%), mean±standard deviation, or median [25th-75th interquartile range], depending on variable distribution.
MR, mitral regurgitation; NS, nonsignificant; NYHA, New York Heart Association; SPPA, systolic pressure of pulmonary artery; STS, Society of Thoracic Surgeons.
MR improved by at least 1 degree according to European guidelines at the 6-month follow-up in 73 patients (50.7%) and the improvement persisted in 69 (47.9%) at 1 year. The sensitivity and specificity of the Multivalvular Score in this population were 0.821 and 0.652, respectively, as shown in Figure 1B (area under the curve=0.772 [95%CI, 0.663-0.881], P <.001). The 6-month mortality rate in these patients was 31.9% compared with 35% in the initial sample (P=NS).
The Multivalvular Score is the first tool fully available for clinical use that has demonstrated a certain capacity to predict the outcome of moderate or severe MR following TAVI. This scenario is often faced by the Heart Team and, until now, only surgical scores have been available. These scores can be used to determine the risk of dual valve replacement but are not useful to select which patients might benefit from more conservative approaches with single aortic valve replacement. Although there are certain limitations regarding the accuracy of the Multivalvular Score, its prospective validation opens a gate to more extensive use that will help to improve the accuracy of this tool, as well as to extend its applicability to alternative scenarios where more than 1 valve is severely affected.5,6
In conclusion, this research adds evidence confirming the constant improvement of MR following TAVI in half of the patients and validates the Multivalvular Score as a simple tool that helps to predict which patients with concomitant AS and moderate or severe MR will improve after isolated TAVI. Conversely, it is also crucial to identify those patients who will require a surgical, percutaneous, or hybrid strategy to repair both valves.
FundingThe project was funded by a grant from the Instituto de Salud Carlos III (PI14/00022) and by the Coronary and Structural Course (CSC).
We thank all the institutions that participated in the development of the Multivalvular Score: Hospital Clínico Universitario San Carlos, Madrid, Spain; Hospital Clínico Virgen de la Victoria, Málaga, Spain; Hospital General Universitario Gregorio Marañón, Madrid, Spain; Hospital Universitario Marqués de Valdecilla, Santander, Spain; Hospital General Universitario de Albacete, Albacete, Spain; and the Quebec Heart and Lung Institute, Quebec, Canada.