Surgical repair of a supracardiac total anomalous pulmonary venous connection (TAPVC) consists of creating an unobstructed anastomosis between the pulmonary venous confluence and the left atrium (LA), ligating the vertical vein (VV), and closing the atrial septal defect. In some patients with obstructive TAPVC and small, noncompliant left-side chambers, the surgical decision not to ligate the VV can help to decompress the high pressure in the left atrium and prevent a pulmonary hypertensive crisis after surgery. However, if the VV remains opened, the left-to-right shunt through the vertical and innominate veins increases with age in relation to reduced diastolic elasticity of the left-side chambers with the consequent deleterious effects, such as right ventricular enlargement and dysfunction, tricuspid regurgitation, and pulmonary hypertension.
We report the first case of an adult patient with a restrictive left ventricle and a partially ligated VV after TAPVC surgery, who underwent a combined percutaneous procedure of closure of the VV with a device before implantation of an atrial flow regulator device to prevent left-sided heart failure. The patient signed the informed consent to publish this report.
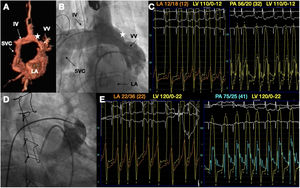
A 62-year-old man with supracardiac TAPVC and atrial septal defect underwent 2-step surgery: first, connection of the pulmonary venous confluence with the LA and closure of the atrial septal defect with patch at the age of 33 years, and secondly, VV ligation at the age of 52 years. In the last visit, the patient reported dyspnea and angina on minimal exertion, and was in New York Heart Association (NYHA) functional class III. Ecocardiography showed enlargement and dysfunction of the right ventricle, severe tricuspid regurgitation, and pulmonary hypertension. Cardiac magnetic resonance and angiography demonstrated the patency of the VV with partial ligation after surgery (figure 1A,B). Hemodynamic data showed mean LA pressure of 12mmHg with V-wave of 18mmHg; left ventricular (LV) pressure of 110/0-12mmHg, and pulmonary artery (PA) pressure of 56/20 (32) mmHg (figure 1C). Qp:Qs was 2.5:1. After transient balloon occlusion (figure 1D), the mean LA pressure rose to 22mmHg (V-wave 36), telediastolic LV pressure to 22mmHg, and PA pressure to 75/25 (41mmHg) (figure 1E). The patient experienced onset of chest pain and breathlessness at that moment. Due to these findings, we planned a 2-step percutaneous procedure, firstly creating a fenestration to descompress the LA with an 8-mm atrial flow regulator (AFR) (Occlutech, Sweden) and secondly closing the VV with an Amplatzer Muscular VSD occluder (AmVSD) (AGA MC, United States).
A: volume rendering 3D cardiac magnetic resonance images showed the partial ligation of the VV (star). B: angiography showed the same structures. C: preprocedure hemodynamic assessment. D: angiogram showing the transient balloon test occlusion of the VV. E: hemodynamic data demonstrated the increase in LA, LV, and PA pressures after balloon test occlusion. IV, innominate vein; LA, left atrium; LV, left ventricle; PA, pulmonary artery; SVC, superior vena cava; VV, vertical vein.
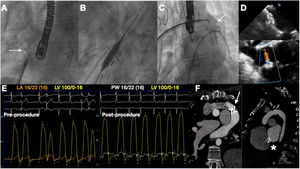
Via the right femoral vein, a transeptal puncture of the patch was performed using an echo and fluoroscopy-guided approach. An 8-mm AFR was implanted and dilated with an 8-mm noncompliant balloon (figure 2A,B). Afterwards, the VV was closed using an 18-mm AmVSD (figure 2C). After VV closure, restrictive flow through the AFR was evident (figure 2D) with no LA pressure elevation (mean 16 with V-wave 22mmHg, before and after the procedure) (figure 2E), with a slight decrease in PA pressure 52/19 (30) and a Qp:Qs: 1.3:1.
A: the arrow marks the 8-mm AFR device implanted in the interatrial septum. B: dilatation with an 8-mm high pressure balloon. C: angiogram showing the VV closure with an 18-mm AmVSD (arrow). D: echocardiogram demonstrating the AFR device correctly implanted on the top, and on the bottom a restrictive flow between the atria through the AFR. E: final hemodynamic result without the increase in LA pressure or pulmonary wedge pressure. F: 2-year-follow-up computed tomography images showing the AmVSD occluding the VV (arrow) and the patent AFR (asterisk). AFR, atrial flow regulator; AmVSD, Amplatzer muscular ventricular septal defect occluder.
The patient made an uneventful recovery and after a 2-year-follow up remained in NYHA I-II functional class and without angina. Computed tomography showed a good result with both devices (figure 2F).
The creation of an interatrial shunt with different devices has been proven feasible in other situations of high LA pressure that lead to pulmonary congestion such as heart failure (HF). Promising results after the implantation of these devices have been reported in pulmonary hypertension and HF patients with preserved and reduced ejection fraction.1,2.Based on studies on the reduction of left-sided cardiac output and pulmonary capillary wedge pressure by creating an interatrial shunt, it has been theoretically proven with a computer simulator in patients with heart failure and mildly reduced or preserved ejection fraction, that the ideal inner fenestration diameter is 8-10mm to decompress the left atrial pressure without a significant increase in Qp:Qs.3 These device sizes were demonstrated to be optimal in the recently published AFR-PRELIEVE TRIAL in patients with heart failure and either preserved or reduced ejection fraction.4
This case demonstrates in vivo that is possible to abolish a high extracardiac left-right shunt and decrease the deleterious effects of pulmonary overflow using a percutaneous device, as well as to prevent left-sided heart failure with a specific fenestrated interatrial device in the presence of a restrictive LV.
FUNDINGNo funding to declare.
AUTHORS’ CONTRIBUTIONSÁ. Sánchez-Recalde, F. Gutiérrez-Larraya, and V. Pascual-Tejerina performed the case. V. Pascual-Tejerina, and Á. Sánchez-Recalde drafted the manuscript. V. Pascual-Tejerina, and J. Ruiz-Cantador collected the images and the follow-up data of the patient. F. Gutiérrez-Larraya, J. Ruiz-Cantador, L Rodríguez-Padial, and J.L. Zamorano critically reviewed the manuscript. All the authors approved the published version of the manuscript.
CONFLICTS OF INTERESTÁ. Sánchez-Recalde is associate editor of Rev Esp Cardiol. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed.