Although uncommon, spontaneous coronary artery dissection (SCAD) is increasingly recognized as a cause of acute coronary syndrome (ACS), particularly in women. It has a different pathophysiology to atherothrombotic ACS, with a favorable outcome after the acute phase and a natural tendency to spontaneous repair of the arterial wall.1 An expectant conservative approach, reserving intervention for patients who are clinically unstable, has been shown to be safe and have good outcomes.2 Data from the Registro Nacional de Disección Coronaria Espontánea (National Registry of Spontaneous Coronary Dissection) show that 80% of patients received conservative management, with good outcomes.3 In addition, intervention in SCAD (initial or after a failed conservative approach) is complex, with results that are not always satisfactory and a high rate of complications.4 We present the outcomes and clinical, angiographic and optical coherence tomography (OCT) follow-up of 3 patients with SCAD who required revascularization, treated with coronary fenestration. The patients gave informed consent for their data collection and subsequent reporting (NCT-03607981).
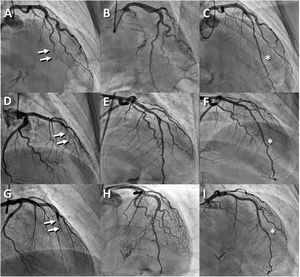
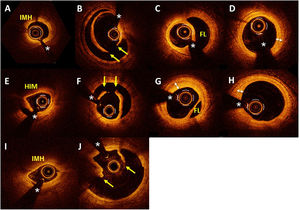
The first case was a 41-year-old woman who was admitted with unstable angina pectoris with ST elevation in the anterior leads. Coronary angiography showed occlusion of the left anterior descending artery (LAD) (figure 1A; ) that, on OCT, corresponded to an intramural hematoma (figure 2A). Given the persistent symptoms and lack of flow, multiple dilatations were performed with a cutting balloon (AngioSculpt 2.5 × 15mm, Spectranetics, USA), with angiographic and clinical improvement (figure 1B; ; OCT findings in figure 2B). At follow-up, the clinical progress was satisfactory and without incident. Follow-up coronary angiography was scheduled for 6 months, which showed images consistent with persistence of the intimal tear in the segment treated with fenestration (figure 1C; ); this was confirmed by OCT, showing a double lumen and diffuse intimal thickening (figure 2C,D).
Optical coherence tomography scan in the acute setting (before and after fenestration) and at follow-up at 6 months. The yellow arrows show the intimal tears. The white double-headed arrows indicate the thickened intima. The asterisks show guidewire artefact. FL, false lumen; IMH, intramural hematoma.
The second case was a 46-year-old woman who was admitted with non--ST-elevation ACS. Coronary angiography was performed when the patient was stable at 48hours. A type 1 SCAD was seen in the mid LAD, with TIMI (Thrombolysis in Myocardial Infarction) 3 distal flow, and we decided to manage conservatively. A few hours after discharge the patient developed further chest pain accompanied by ST-segment elevation in the anterior leads. Urgent coronary angiography showed deterioration in coronary flow (TIMI 1) (figure 1D). OCT confirmed an intramural hematoma (figure 2E) which was treated with dilatation using a cutting balloon (AngioSculpt 2.5 × 8mm). Flow then recovered to TIMI 3 (figure 1E) and the pain disappeared. OCT showed multiple fenestrations (figure 2F). Repeat coronary angiography at the 6-month follow-up showed a localized intracoronary filling defect indicative of a residual intimal tear in the fenestrated segment (figure 1F), with good flow. OCT confirmed persistence of the localized dissection and intimal thickening in this area (figure 2G,H).
The third case was a 43-year-old woman who was admitted with ACS with ST elevation in V1 to V3. Urgent coronary angiography revealed an occlusion of the LAD (figure 1G) and OCT confirmed an intramural hematoma (figure 2I). Multiple dilatations were performed with a cutting balloon (AngioSculpt 2 × 20mm), until there was restoration of TIMI 3 flow (figure 1H) and signs of successful fenestration on OCT (figure 2J). Coronary angiography at 6 months showed the persistence of images consistent with residual intimal tear, with good flow in the previously treated area (figure 1I). As the angiographic image was diagnostic of residual dissection, and the vessel was relatively small, we decided not to perform OCT.
There is increasing evidence that coronary intramural hematoma is the initial pathophysiological event in SCAD.5 The increase in intramural pressure would cause compression of the lumen and myocardial ischemia. Tearing of the intimal layer would therefore provide a natural “escape” for the hematoma, with formation of the typical double lumen image, release of intramural pressure and improvement in coronary flow. In patients with SCAD who require intervention, it is common to find intramural hematoma without the double lumen.3,4 Fenestration with a cutting balloon has been shown to be an effective therapeutic alternative to achieve transformation of the parietal hematoma in cases of SCAD with a double lumen, improving coronary flow and achieving clinical stabilization. This strategy means stent implantation can be avoided.
This article is the first to report a series of consecutive patients with invasive treatment of SCAD using coronary fenestration with systematic follow-up. The initial results and mid-term clinical outcomes have been excellent. However, at follow-up, we observed the persistence of localized residual dissection and diffuse intimal thickening in the treated segment. These findings indicate that the vascular repair was not complete (restitutio ad integrum), as is usual in patients managed conservatively. Further studies will be needed to determine the clinical implications of these new findings and whether the postfenestration vascular repair phenomenon is incomplete or simply takes much more time.
FUNDINGNone.
AUTHORS’ CONTRIBUTIONSAll the authors contributed substantially to the conception and design, data collection or analysis and interpretation, wrote or critically reviewed the article for intellectual content, gave approval of the final version of the article for publication, and agree to accept responsibility for all aspects of the article and to investigate and resolve any questions related to the accuracy or trueness of any part of this work.
CONFLICTS OF INTERESTNone of the authors have any conflicts of interest in relation to this article.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.recesp.2021.07.010