An 88-year-old man with a history of biological aortic valve replacement, pacemaker implantation and chronic atrial fibrillation with thromboembolic protection (dabigatran 110mg x 2) was admitted for serious intestinal bleeding. Bowel angiodysplasia was diagnosed and the anticoagulation therapy was discontinued. The patient was scheduled to undergo endovascular left atrial appendage (LAA) closure with the Amplatzer Amulet device (St Jude Medical)1 given that the patient had a score of 4 on both the HAS-BLED and CHA2DS2-VASc scales. After sheath insertion in the right femoral vein, a 0.035″ conventional J-tip wire repeatedly crossed to the left side of the spine. Contrast media injection confirmed the absence of a right inferior vena cava (IVC) and showed a left IVC combined with a hemiazygos continuation (Figure 1), confirmed by computed tomography angiography (Figure 2). Consequently, the procedure was aborted and finally cancelled. Of note, the transgastric IVC long-axis view by transesophageal echocardiography showed the hepatic veins and strongly suggested an IVC interruption (Figure 1).
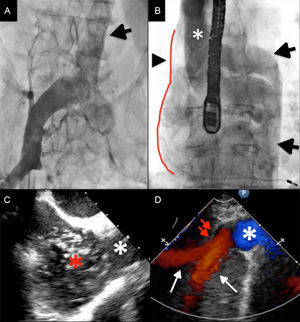
A: Venography showing a left IVC (arrow) and the absence of the right IVC. B: Hemiazygos continuation (2 arrows) and, due to the azygos cross (asterisk), the inferior systemic venous return enters the superior vena cava (arrow head and limited by the red line). C: Transgastric IVC long-axis view by transesophageal echocardiography. Superior vena cava (white star); microbubbles in the left atrium coming from the superior vena cava after injection in the left IVC (red star). D: IVC (white star), hepatic veins (white arrows); IVC interruption (red arrows). IVC, inferior vena cava.
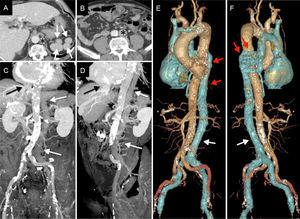
Computed tomography angiography. A: Polysplenia (arrows), hypertrophy of the hemiazygos vein (asterisk). B: Absence of IVC on the right and left position of the IVC (asterisk). Coronal (C) and sagittal reconstructions (D) showing the interruption of IVC (black arrow) with hemiazygos continuation and left-sided IVC (white arrows). E and F: Volumetric rendering images showing the abnormal systemic venous return from the lower body with a left-sided IVC (white arrow) and a hemiazygos continuation (red arrow). IVC, inferior vena cava.
All isolated congenital variations of the IVC are a consequence of abnormal embryologic development, affecting approximately 4% of the population.2 Because of the wide variety of anomalous persistence, regression, or anastomoses between vitelline, posterior cardinal, subcardinal, and supracardinal veins, several congenital abnormalities may exist alone or in combination.2 The most frequent are double IVC (0.2%-3%), azygos and hemiazygos continuation of the IVC (0.6%), and left-sided IVC joining the left renal vein (0.2%-0.5%).2,3 Indeed, more than 1 anomaly can coexist, such as in our patient, in whom the left-sided IVC was combined with an interrupted right IVC and hemiazygos continuation. These 2 rare combined abnormalities resulted in an abnormal lower systemic venous return via the azygos venous system to the superior vena cava. In addition to the abnormal venous return, polysplenia (Figure 2) was diagnosed and enabled the complex diagnosis of left isomerism syndrome. Indeed, azygos and hemiazygos continuation of the IVC has been associated with situs anomalies, asplenia or polysplenia, and congenial heart malformations.3,4
The consequence of our patient's venous anomalies was a circuitous and abnormally long trajectory to the heart from the femoral approach, and thus the failure of endovascular LAA closure. In such anatomies or in the absence of patent IVC, transjugular or subclavian approaches may be challenging alternatives considering the transseptal puncture and LAA cannulation. Other approaches such as thoracoscopic appendage exclusion may also be considered, but our 88-year-old patient refused any further procedures.5 Of note, in a similar anatomy, only 1 successful right-sided catheter ablation has been described in a child using the transfemoral approach.6
Although often asymptomatic, IVC congenital variations are an important condition to recognize before or during any endovascular procedure such as structural interventions (eg, MItraClip, LAA closure), electrophysiological interventions or IVC filter insertion.