Traditionally, the CHADS2 score has been employed for thromboembolic risk stratification in patients with nonvalvular atrial fibrillation (AF).1 However, with this scoring system, the basis for decisions on antithrombotic therapy was poorly defined in a large proportion of patients with intermediate thromboembolic risk, since antiplatelet and anticoagulation therapy are considered equally valid options.1 However, it is evident that the implications of the 2 treatments differ and that, within the group of intermediate risk patients, not all of them have the same degree of risk. In this context, the CHA2DS2-VASc score, which is a more complete scale since it includes other factors that modulate thromboembolic risk, enables better identification of those patients with AF who will most benefit from anticoagulation therapy2 than the CHADS2 score. In fact, the guidelines of the European Society of Cardiology recommend its use in clinical practice.2 A number of studies have shown that the use of the CHA2DS2-VASc score enables more accurate reclassification of these patients.3 However, in routine clinical practice, the criteria for anticoagulation in accordance with this score are less well known.
The objective of this study was to determine whether there are differences in the use of antithrombotic therapy depending on the application of the CHA2DS2-VASc or CHADS2 risk scores. For this purpose, we analyzed the data of the Val-FAAP study, classifying the patients according to the CHA2DS2-VASc score. The Val-FAAP study was a multicenter, cross-sectional trial carried out in the primary care setting, in which each investigator was required to enroll a total of 4 consecutive patients who met the following inclusion criteria: age 18 years or over, patients of both sexes, and patients with a previous electrocardiographic diagnosis of AF.4
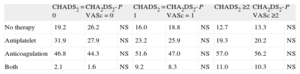
The Val-FAAP study included a total of 3287 subjects with AF (mean age, 71.9 [10.1] years; 52.3% men; 92.6% with a history of hypertension; 21.3% with heart failure; and 20.9% with ischemic heart disease). Of the overall group of patients, 4.5% had a CHADS2 score of 0; 28.1%, a score of 1; and 67.4%, a score of 2 or higher. When the CHA2DS2-VASc score was used, these rates were 1.9%, 12.4%, and 85.7%, respectively. The Table indicates the percentages of patients according to the antithrombotic therapy they received and the thromboembolic risk stratification score.
Distribution of Patients (%) According to the Antithrombotic Therapy Received and Thromboembolic Risk Stratification Score
| CHADS2 = 0 | CHA2DS2-VASc = 0 | P | CHADS2 = 1 | CHA2DS2-VASc = 1 | P | CHADS2 ≥2 | CHA2DS2-VASc ≥2 | P | |
| No therapy | 19.2 | 26.2 | NS | 16.0 | 18.8 | NS | 12.7 | 13.3 | NS |
| Antiplatelet | 31.9 | 27.9 | NS | 23.2 | 25.9 | NS | 19.3 | 20.2 | NS |
| Anticoagulation | 46.8 | 44.3 | NS | 51.6 | 47.0 | NS | 57.0 | 56.2 | NS |
| Both | 2.1 | 1.6 | NS | 9.2 | 8.3 | NS | 11.0 | 10.3 | NS |
NS, not significant.
The main results of our study show patient distribution according to the CHA2DS2-VASc score compared with that corresponding to the CHADS2 score. In principle, this enables the identification of the patients who will benefit most from long-term anticoagulation therapy for the prevention of thromboembolic complications; according to the CHA2DS2-VASc score, the vast majority of patients with AF are at high thromboembolic risk. These data are in line with those reported in different populations, in which thromboembolic risk stratification has been shown to be more accurate with the CHA2DS2-VASc score than with the CHADS2 score, mainly in patients with intermediate thromboembolic risk.3
Unfortunately, antithrombotic therapy is improperly applied.5,6 For example, more than 40% of patients with a CHADS2/CHA2DS2-VASc score of 0 receive oral anticoagulation therapy and more than 30% of those with a CHADS2/CHA2DS2-VASc score of 2 or higher do not. This has several implications. On the one hand, the relative lack of definition of the CHADS2 score with respect to the embolic risk of patients with scores of 0 or 1 is not the reason for the deviation of the indication for anticoagulation from the standard guidelines, since reclassification using the CHA2DS2-VASc score, which is more accurate in this risk range, continues to show that the anticoagulation regimen is inadequate. On the other hand, while it is true that the risk of bleeding in patients with a CHADS2/CHA2DS2-VASc score of 2 or higher has not been analyzed, it would be difficult to explain such a high rate of underuse of anticoagulation therapy by an excessive risk of hemorrhage. Although the underuse of anticoagulation therapy in patients with AF had previously been demonstrated,5 the data from this study indicate, first, that in Spain, there is a great deal of room for improvement in antithrombotic therapy to prevent stroke risk in patients with AF and, second, that this shortfall is independent of the risk score employed.
All in all, in Spain, therapy for the prevention of thromboembolic complications is not properly applied, and its prescription appears to be independent of the risk stratification score employed. These data lend further support for the need to raise awareness among primary care physicians in Spain of the importance of familiarity with and more extensive use of risk stratification scores and of the correct application of thromboembolic therapy.