To the Editor,
Given the complex anatomy of the left atrium (LA) and pulmonary veins (PVs), physicians should obtain individualized information on patient anatomy prior to atrial fibrillation (AF) ablation. Magnetic resonance imaging (MRI) is an excellent tool in anatomic reconstruction. Furthermore, three-dimensional (3D) navigation systems (NS) are widely used.1, 2
Radiologic rotational angiography (RRA) creates a 3D reconstruction of the cardiac chambers during the ablation procedure. It has previously been compared with imaging tests3, 4, 5 but not with 3D NS.
We propose to evaluate the precision of RRA in LA and PVs reconstruction and compare it with that offered by using MRI and 3D NS.
We enrolled consecutive patients indicated for AF ablation. Exclusion criteria were bronchial asthma, obesity preventing free radiologic arm rotation, difficulty in transseptal puncture, kidney failure, and iodine allergy. Ablation was performed under general anesthesia and with Ensite-NavX® 3D NS (St. Jude Medical)3; cardiac MRI (Philips Achieva® 3T) had been performed previously. We programmed 240° C-arm rotation (Philips Allura equipment). High-dose adenosine was injected (18mg-24mg) to provoke a transient pause due to atrioventricular block. Once the block had started, iodine contrast was injected into the LA and the programmed rotation was conducted. Postprocessing of the images rendered a 3D LA reconstruction. One researcher (CH) analyzed the reconstruction blind and compared MRI (number of PV and diameter of PV ostia) with the 3D NS (number of PVs).
Continuous variables are described as median [interquartile range] and compared with the Wilcoxon signed-rank test. Correlation was calculated with Spearman's coefficient.
Initially, we enrolled 22 patients; 5 were excluded (2 for obesity, 1 for difficulty in transseptal puncture, 1 for asthma, and 1 for kidney failure). RRA was performed with no complications in 17 patients; 2 in the pilot phase, leaving 15 who constituted our study group (Table 1).
Table 1. Baseline Characteristics.
| Patients | 15 |
| Age, years | 52±10 |
| Men | 14 (93) |
| LVEF, % | 63±9 |
| Indication for ablation | |
| Paroxystic AF | 13 (86.7) |
| Persistent AF | 2 (13.3) |
| Rhythm at RRA | |
| Sinus rhythm | 10 (67) |
| AF | 5 (33) |
AF, atrial fibrillation; LVEF, left ventricular ejection fraction; RRA, radiologic rotational angiography.
Data are expressed as no. (%) or mean±standar deviation.
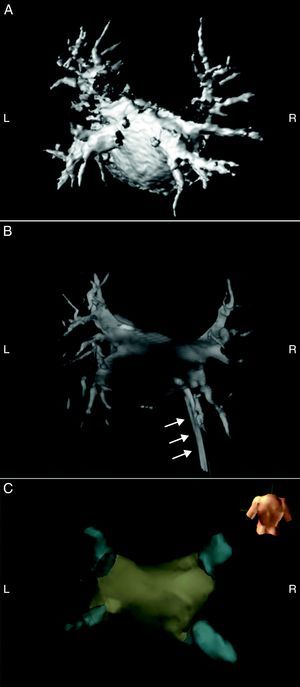
In 3 patients, RRA images could not be analyzed. In these patients, pause duration was too short for analysis, 2.1 [1.2-4.8] vs 12.3 s [7.8-16.2] (P=.034). The RRA enabled us to observe 4 PVs with independent ostia in 8 of 12 patients with images suitable for analysis, and common antra in 4. When compared with 3D NS, RRA identified the same number of PVs and common antra in 10 of 12 patients (Figure 1). In the remaining patients, 3D NS showed 1 left common antrum and 1 intermediate right PV missing in RRA and MRI.
Figure 1. Magnetic resonance imaging reconstruction of left atrium (A), rotational radiologic angiography (B) and Ensite-NavX® (C). Posterior view. Note in B the catheters and sheaths penetrating into the left atrium (arrows). L, left; R, right.
MRI and measurements were available for 10 patients and identification of PVs and common antra proved the same as in RRA in 9 of them (Figure 1). In the one remaining patient, MRI identified 1 left intermediate PV that RRA did not. PVs diameter was 14mm (14-17.3) in MRI and 14.8mm (14.1-17.7) in ARR, and we obtained a statistically significant positive correlation (rs=0.722; P<.001).
RRA offers precise identification of LA anatomic structures provided the postadenosine pause is significant. In a minority of patients, this cannot be achieved.
Our study is consistent with other publications in that the pause duration was decisive for RRA images to be suitable for analysis.3, 4, 5 This is probably because the relaxation following ventricular contraction drains contrast towards the ventricle and reduces the intensity of atrial opacification. We were able to identify PVs and measure PV diameter accurately. We coincide with other authors5 in finding that RRA slightly overestimates diameters, perhaps because of distension caused by the contrast injection or atrial cycle phase changes.
We also compared RRA with 3D NS. A recently published study randomized patients to 3D NS or RRA during PV ablation.6 However, we have found no publication that compares methods in the same patient. In our study, identification of PVs and common antra using both methods was identical in all except 2 cases. In these patients, RRA was concordant with MRI, suggesting it is more accurate than 3D NS.
The use of high-dose adenosine suggests general anesthesia is needed. Although neither our study nor others have found complications with this method, its safety in patients with structural heart disease has not been determined. RRA could not be used in 5 patients, but in 4 of them this limitation could have been identified earlier, thus permitting the use of a different imaging method.
In conclusion, intraoperative RRA of the LA provides anatomic information crucial to AF ablation provided there is always a significant pause secondary to adenosine.
CONFLICTS OF INTERESTDr Almendral has received lecture fees from St. Jude Medical and his institution has received payment from St. Jude Medical for educational presentations.
.
Corresponding author: almendral@secardiologia.es