Between 1992 and 1997,1 a valvular heart disease similar to that produced by carcinoid tumors associated with fibrosis, leaflet retraction, and calcification was reported in patients treated with ergotamine derivatives (fenfluramine-phentermine). The activation of 5-hydroxytryptamine (serotonin) 2B (5-HT2B) receptors, which are highly abundant in the valvular endocardium, through signaling pathways mediated by Src kinases, stimulates fibroblast mitogenesis, with increased extracellular matrix production. It also causes the histological changes typical of this restrictive valvular heart disease, referred to as fen-phen since it was first described.2 In recent years, the development of this type of valvular heart disease has also been reported in patients with Parkinson's disease treated with dopamine agonists3 and, more recently, specifically with the administration of cabergoline in the treatment of hyperprolactinemia, in which lower doses are utilized.4–6
Our aim was to evaluate the prevalence of valvular heart disease in a group of patients with hyperprolactinemia and compare it with the incidence in a control group of healthy volunteers who worked in our center. Patients from the neuroendocrinology unit who had been undergoing active treatment with cabergoline for at least 6 months prior to inclusion in the study were consecutively enrolled. Both the cumulative dose received and the duration of treatment were also evaluated in these patients. The study of valvular heart disease was carried out by means of echocardiography to rate the presence of regurgitation and stenosis as insignificant, mild, moderate, or severe in accordance with the recommendations of the European Society of Cardiology guidelines. In the morphological examination, the mitral valve tenting area was considered to be an indicator of restricted valve closure (cm2), a thickening greater than 5mm in leaflets or annulus was considered to be indicative of disease, and the presence of calcifications anywhere in the valve or subvalvular apparatus was evaluated qualitatively. For the statistical analysis, we used the Student t test for the comparison of means or the chi-square test for the comparison of proportions, and logistic regression analysis was performed to correlate the presence of valvular heart disease with the duration of treatment and the cumulative dose. Patients with previously diagnosed valve or heart disease were excluded from both groups.
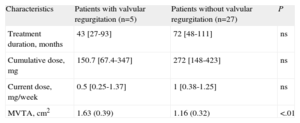
In all, 32 patients with hyperprolactinemia of any origin were compared with 32 healthy controls. Seventy-five percent of the patients and 65% of the controls were women, with a more advanced mean age in the control group (38.78 [10.4] years vs 46.68 [12.5] years; P=.008) and a similar distribution of cardiovascular risk factors (hypertension, diabetes mellitus, dyslipidemia, and smoking habit) in both groups. The majority of the patients had hyperprolactinemia due to microprolactinoma (42%). With respect to the doses of cabergoline administered, the median cumulative dose was 158mg [interquartile range, 69-363mg] and the median dose received at the time of enrollment was 0.5mg/week [0.25-1.25mg/week], with a median treatment duration of 46 months [30-96 months]. Severe valvular disease was not found in either of the groups and none of the patients had symptoms of heart disease. Five of the patients treated with cabergoline (Table 1) had valvular heart disease which was mild or worse (15%); 1 of these patients had concomitant mitral and tricuspid valve involvement, but did not differ from the remaining patients in terms of current dose, cumulative dose, or treatment duration. The mitral valve tenting area was significantly greater in these 5 cases compared to the remaining 27 (1.63 [0.39] cm2 vs 1.16 [0.28] cm2; P=.003). We found no differences between the 2 groups with respect to type of valve disease (Table 2) and, on comparing the 5 hyperprolactinemic patients with the 11 controls who had mild valvular heart disease or worse, the mitral valve tenting area tended to be greater in the treated patients, a trend that was not significant (1.63 [0.39] cm2 vs 1.30 [0.27] cm2; P=.07). There was only 1 report of moderate valvular heart disease in the patient group: a case of moderate tricuspid regurgitation in a 22-year-old woman who had been treated for 53 months for microprolactinoma, with a cumulative dose of 130mg. The valve showed no evidence of thickening or calcification.
Comparison Between Hyperprolactinemic Patients With and Without Valvular Regurgitation.
| Characteristics | Patients with valvular regurgitation (n=5) | Patients without valvular regurgitation (n=27) | P |
| Treatment duration, months | 43 [27-93] | 72 [48-111] | ns |
| Cumulative dose, mg | 150.7 [67.4-347] | 272 [148-423] | ns |
| Current dose, mg/week | 0.5 [0.25-1.37] | 1 [0.38-1.25] | ns |
| MVTA, cm2 | 1.63 (0.39) | 1.16 (0.32) | <.01 |
MVTA, mitral valve tenting area; ns, not significant.
Data are expressed as median [interquartile range] or mean (standard deviation).
Comparison of the Prevalence of Valvular Heart Disease in Patients and Controls.
| Valvular regurgitation | Patients | Controls | P |
| MR (Yes/No) | 7 (22)/25 | 19 (59)/13 | .044 |
| Insignificant | 5 (15) | 11 (34) | .034 |
| Mild | 2 (6.25) | 7 (21) | ns |
| Moderate | 0 | 1 (3) | ns |
| Severe | 0 | 0 | ns |
| AR (Yes/No) | 1 (3)/31 | 1 (9)/29 | ns |
| Insignificant | 0 | 0 | ns |
| Mild | 1 (3) | 1 (3) | ns |
| Moderate | 0 | 0 | ns |
| Severe | 0 | 0 | ns |
| TR (Yes/No) | 20 (62.5)/12 | 16 (50)/16 | ns |
| Insignificant | 17 (53) | 12 (37.5) | ns |
| Mild | 2 (6.25) | 4 (12.5) | ns |
| Moderate | 1 (3) | 0 | ns |
| Severe | 0 | 0 | ns |
| PR (Yes/No) | 3 (9)/29 | 4 (9)/28 | ns |
| Insignificant | 3 (9) | 3 (6) | ns |
| Mild | 0 | 0 | ns |
| Moderate | 0 | 1 (3) | ns |
| Severe | 0 | 0 | ns |
| Valvular thickening, calcification, fibrosis (Yes/No) | 0 | 4 (12.5)/282 aortic2 mitral | ns |
| MVTA, cm2 | 1.63±0.39 | 1.30±0.27 | ns |
AR, aortic regurgitation; MR, mitral regurgitation; MVTA, mitral valve tenting area; ns, not significant; PR, pulmonary regurgitation; TR, tricuspid regurgitation.
Data are expressed as No. (%) or mean±standard deviation.
The results of our study agree with current opinion drawn from other reports4,5 and a review recently published in the Revista Española de Cardiología.6 At the doses administered in the treatment of hyperprolactinemia, cabergoline is not associated with an increase in the development of valvular heart disease in our general population. One limitation we should point out is the small sample size and the fact that the echocardiographic study of the patients was unblinded. In accordance with other authors, we found no relationship to the treatment dose or duration, but the low number of events may have had an influence on the findings. With respect to the mitral valve tenting area, it could be a useful parameter for predicting the development of valve disease, and its inclusion in the follow-up study could provide us with further information in this respect. We can conclude that, at the present time, it would be wise to perform an echocardiographic examination prior to the initiation of treatment and yearly thereafter; discontinuation of treatment does not appear to be indicated in the case of insignificant valve disease, as it will probably take a long time for a more severe condition to develop, but perhaps cabergoline should be replaced by another drug in the case of significant valvular heart disease. Prospective studies involving a larger number of patients are needed before we can draw any firm conclusions.
.