.
Dextrocardia occurs in 1/12 000 pregnancies, of which approximately a third are associated with inversion (mirror imaging) of the other visceral organs (situs inversus totalis).1 In these cases, inversion of the normal anatomy can hamper the performance of fluoroscopy-guided interventional procedures.
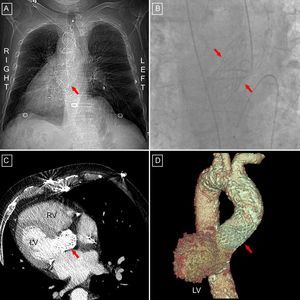
We describe a 78-year-old man with situs inversus totalis and symptomatic severe aortic stenosis who was referred to our hospital for transcatheter implantation of an aortic valve. The patient had previously been considered ineligible for conventional aortic valve replacement due to high surgical risk (EuroSCORE logistic, 21%; porcelain aorta). The procedure was performed using a right femoral approach but was complex due to inversion of the cardiac anatomy. Classic ventriculography with 5 segments was performed using a 30° left oblique projection (the usual view is a 30° right oblique projection); a 10° caudal and a 10° right oblique projection were used to align the 3 Valsalva sinuses. Following aortic valvuloplasty with ventricular overdrive pacing, a 29-mm CoreValve® self-expanding aortic valve prosthesis (Medtronic, Irvine, California, United States) was successfully implanted. The patient was stable and asymptomatic when returned to the coronary unit. However, 24 h later he experienced cardiac tamponade secondary to right ventricular free wall perforation by the temporary pacemaker lead and required surgery. Three days later the patient experienced high-grade atrioventricular block and consequently a permanent dual-chamber pacemaker was implanted. The patient was discharged 10 days later, with no further incidents (Figure).
Dextrocardia is a rare abnormality of the heart position.2 Most cases with situs solitus are associated with other cardiac or noncardiac malformations. However, patients with situs inversus totalis (as in our patient) rarely have other associated malformations1-3 and, therefore, it is not unusual them to reach older ages in which degenerative aortic stenosis is common.
Inversion of cardiovascular structures is an added procedural difficulty for percutaneous aortic valve implantation.4 The most important difficulties are related to stable positioning of the temporary pacemaker when crossing the aortic valve with the straight guidewire or attempting to align the 3 Valsalva sinuses to assess correct positioning of the prosthesis. In fact, our patient experienced late perforation by the pacemaker leads, possibly related to malpositioning. In cases such ours, in which the abnormal cardiac anatomy can affect the operator's spatial orientation, we recommend careful catheter handling and conscientious selection of the angiographic projections (usually opposite to those seen in a patient with levocardia5). To our knowledge, this is the first case of the implantation of a CoreValve aortic valve prosthesis in a patient with situs inversus totalis.