Study of the response to antiplatelet agents in daily clinical practice has reached a decisive moment. We are increasingly convinced that measuring platelet response to antiplatelet agents may help in risk stratification1–3; however, as recent negative studies have shown,4,5 serious reservations remain about using risk stratification to justify a change in antiplatelet treatment. Research in this area has mainly focused on resistance to adenosine diphosphate blockers, fundamentally clopidogrel, possibly because alternative therapeutic approaches are available. Thus, from our perspective, resistance to salicylates has rather been “forgotten” in cardiology.
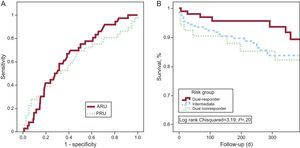
We aimed to study the comparative value of measuring salicylate response (vs response to adenosine diphosphate blockers) in patients with ischemic heart disease. From October 2010 through October 2011, we prospectively enrolled all patients (n=322) with ischemic heart disease —a) acute coronary syndrome, defined as typical chest pain and elevated necrosis markers or T wave/ST segment abnormalities, and b) chronic stable angina, with an objective test of ischemia) receiving a salicylate plus clopidogrel/prasugrel≥4h after the loading dose (≥2h for prasugrel), referred for cardiac catheterization. In each patient, VerifyNow® was used to determine adenosine diphosphate receptor antagonist reactivity (measured in P2Y12 reactivity units [PRU] and arachidonic acid reactivity (measured in aspirin reaction units [ARU]. The definition of a “poor responder” was obtained from the manufacturer's recommendations as opposed to consensus documents (ARU>550U, PRU>235U).6 During the follow-up, the principal variable was the combination of unstable angina (requiring admission), acute myocardial infarction, death (from any cause), stroke, and (angiographically confirmed) stent thrombosis. We obtained follow-up data on 300 patients (93.2%) for a median 247days. We constructed a ROC (receiver operating characteristic) curve for ARU and PRU, and calculated the area under the curve, sensitivity, specificity, predictive values, likelihood ratios and test efficacy for predefined cutoff points. Using the Kaplan-Meier method, patients were stratified in 3 groups: nonresponders, who did not react to any antiplatelet agent; responders, who reacted to 1; and double-responders, who reacted to 2. Data analysis was performed with SPSS 15.0 and a purpose-designed macro.
The mean age was 66±11 years and two thirds were men. Most patients had acute coronary syndrome (96%) and nearly two thirds had elevated myocardial necrosis markers; 40.4% had diabetes, 28.9% were active smokers, and 6.8% had chronic kidney failure. The most frequent diagnosis was acute coronary syndrome without persistent non-ST segment elevation (68.8%). A total of 99.1% were receiving clopidogrel (67.4% with a previous loading dose, mostly 300mg [90.5%]) and 98.8% were receiving acetylsalicylic acid (58.9% with a previous loading dose, mostly 300mg [75.7%]). We recorded 36 events (12 deaths, 12 episodes of unstable angina, 4 myocardial infarctions, 5 cases of stent thrombosis, and 3 strokes).
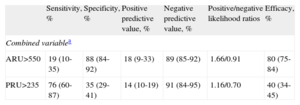
The ROC analysis, with the combination of adverse events as the state variable, indicated that discrimination of the ARU and PRU variables was moderate and that the 2 were very similar; differences were nonsignificant (Figure, panel A; area under the ROC curve for ARU=0.656; 95% confidence interval [95%CI], 0.567-0.744; area under the curve for PRU=0.611; 95%CI, 0.501-0.722). The Table shows the good sensitivity and negative predictive value of PRU, although specificity and positive predictive values were poor. By contrast, ARU gave good specificity and negative predictive values, whereas sensitivity and positive predictive values were low. Likelihood ratios indicated ARU was more effective than PRU at confirming the occurrence of adverse events and was slightly worse at confirming their absence. Finally, efficacy was significantly better with ARU than PRU (80% vs 40%; P<.05).
Comparative Diagnostic Performance of Aspirin Reaction Units vs P2Y12 Reactivity Units
| Sensitivity, % | Specificity, % | Positive predictive value, % | Negative predictive value, % | Positive/negative likelihood ratios | Efficacy, % | |
| Combined variablea | ||||||
| ARU>550 | 19 (10-35) | 88 (84-92) | 18 (9-33) | 89 (85-92) | 1.66/0.91 | 80 (75-84) |
| PRU>235 | 76 (60-87) | 35 (29-41) | 14 (10-19) | 91 (84-95) | 1.16/0.70 | 40 (34-45) |
ARU, aspirin reaction units (resistance to acetylsalicylic acid); PRU, P2Y12 reaction units (resistance to adenosine diphosphate receptor blockers).
In parentheses we show the 95% confidence interval calculated by the Wilson method.
We found 98 (30.4%) dual responders and 188 (58.4%) single responders; of these 188 patients, 179 (95.2%) were poor responders to clopidogrel. There were 36 (11.2%) dual nonresponders. The Kaplan-Meier curve (Figure, panel B), shows that the clinical course was more favorable—although not significantly so—in responders to the 2 antiplatelet drugs than in patients with resistance to 1 or both, with no apparent difference between the drugs, indicating minimal additive value.
Our data indicate that, as a prognostic instrument, measuring ARU is at least as effective as measuring PRU in patients with ischemic heart disease—mainly acute coronary syndrome. Moreover, the consensus cutoff point for ARU has substantially greater general efficacy than that of PRU. Further larger-scale studies are needed to confirm these findings.
FUNDINGThe present study was financed through FFIS-Caja Murcia grant 10/006.
.