SEC 2013 - El Congreso de las Enfermedades Cardiovasculares
6018. Insuficiencia cardiaca/Disfunción ventricular
6018-592.1. MELD Scoring as a Predictor of Outcomes in Patients Presenting with Acute Decompensated Heart Failure
Background: The MELD scoring system, developed in patients with hepatic cirrhosis awaiting liver transplantation, may provide information in HF patients by assessing the degree of renal and hepatic dysfunction. The use of MELD scoring has recently been utilized in ambulatory heart failure patients but has not been put to use in the acute setting. In this study we chose to use the MELD-XI score to evaluate patients admitted with ADHF, because MELD-XI eliminates spuriously elevated INR secondary to anticoagulation agents.
Objective: The goal of this analysis was to assess the association between the Model of End-stage Liver Disease-eXcluding INR (MELD-XI) scoring system and clinical outcomes among patients admitted with acute decompensated heart failure (ADHF).
Methods: We conducted a post hoc analysis using data from the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) trial, a large multicenter trial of patients with ADHF treated with therapy guided by pulmonary artery catheters or therapy guided by clinical assessment. Among 346 individuals, we analyzed the association between admission MELD-XI scores and a composite endpoint of death, re-hospitalization, or heart transplant (Htx). Baseline MELD-XI scores were categorized by tertile values (< 27.4 vs ≥ 27.4 to < 33.2 vs ≥ 33.2) and by dichotomization (< 39 vs ≥ 39) determined by a classification and regression tree (CART) analysis, a nonparametric data-mining tool that can segment data into meaningful subgroups.
Results: Patients in the highest tertile of MELD-XI scores exhibited a significant 32% increased risk (Hazard Ratio [HR] = 1.32; 95%CI 1.11-1.58) for re-hospitalization/death/Htx compared to the first two tertiles. Additionally, the highest tertile was associated with significantly lower 6-month event-free survival (31%) compared to patients in the first and second tertile (49% and 48%, respectively; p = 0.002) (fig. 1). When the MELD-XI data was dichotomized, patients with MELD-XI score #> 39 (observed in 15% of patients) were associated with a significantly increased risk of clinical events (HR = 1.86; 95%CI 1.31-2.64) and a lower 6-month event-free survival (23%) compared to the patients with a lower MELD score (46%; p < 0.001) (fig. 2).
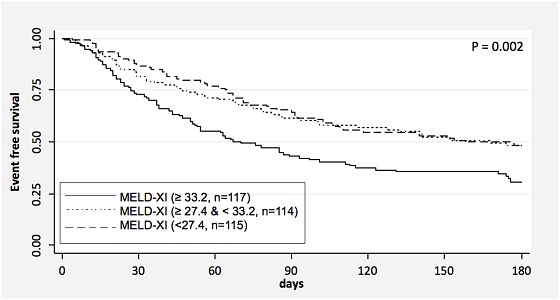
Figure 1. Kaplan-Meier survival curve for composite endpoint (death, cardiac re-hospitalization, and Htx) stratified by admission MELD-XI score tertiles.
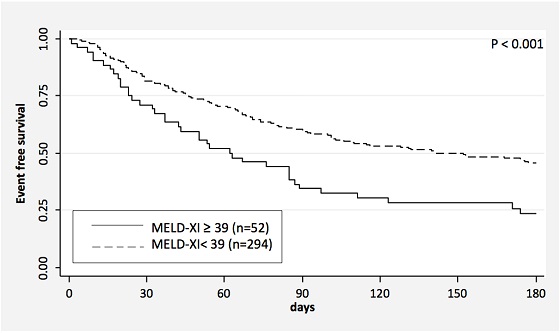
Figure 2. Kaplan-Meier survival curve for composite endpoint (death, cardiac re-hospitalization, and Htx) stratified by dichotomized admission MELD-XI scores.
Conclusions: Not only did we find a large percentage of patients had very elevated MELD-XI scores, but we also found these higher scores to be associated with poor survival and greater risk of clinical events. This study suggests that admission MELD-XI scoring could be utilized as a predictor of survival and risk of clinical events in patients undergoing treatment of acute decompensated heart failure.
Comunicaciones disponibles de "Insuficiencia cardiaca/Disfunción ventricular"
- 6018-554. Estratificación del riesgo de muerte en pacientes con insuficiencia cardiaca mediante árboles de clasificación y regresión
- Josep Lupón Rosés, Marta de Antonio Ferrer, Amparo Galán Ortega, Mar Domingo Teixidó, Roser Cabanes Sarmiento, Elisabet Zamora Serrallonga, Crisanto Díez Quevedo y Antoni Bayes-Genis del Hospital Universitari Germans Trias i Pujol, Badalona (Barcelona).
- 6018-555. Filtrado glomerular renal estimado con la nueva ecuación CKD-EPI-creatinina-cistatina-C y pronóstico a largo plazo en insuficiencia cardiaca crónica
- Elisabet Zamora Serrallonga1, Josep Lupón Rosés1, Marta de Antonio Ferrer1, Joan Vila Domenech2, Judith Peñafiel Muñoz2, Amparo Galán Ortega1, Agustín Urrutia de Diego1 y Antoni Bayes-Genis1 del 1Hospital Universitari Germans Trias i Pujol, Badalona (Barcelona) y 2IMIM, Barcelona.
- 6018-556. Frecuencia cardiaca y calidad de vida en función del ritmo (sinusal o fibrilación auricular) en pacientes con insuficiencia cardiaca
- Marta de Antonio Ferrer, Josep Lupón Rosés, Roser Cabanes Sarmiento, Beatriz González Fernández, Lucía Cano Sanz, Agustín Urrutia de Diego, Mar Domingo Teixidó y Antoni Bayes-Genis del Hospital Universitari Germans Trias i Pujol, Badalona (Barcelona).
- 6018-557. Calidad de vida y fragilidad en pacientes ambulatorios con insuficiencia cardiaca
- Paloma Gastelurrutia Soto, Josep Lupón Rosés, Marta de Antonio Ferrer, Beatriz González Fernández, Roser Cabanes Sarmiento, Lucía Cano Sanz, Agustín Urrutia de Diego y Antoni Bayes-Genis del Hospital Universitari Germans Trias i Pujol, Badalona (Barcelona).
- 6018-558. Relación entre los niveles de presión arterial pulmonar y resultados adversos en la insuficiencia cardiaca aguda descompensada
- Irene Rilo Miranda1, Juan Ramón Beramendi Calero1, José Juan Onaindia Gandarias2, Miren Morillas Bueno2, Susana García Gutiérrez2, Annette Unzurrunzaga Garate2, Kattalin Echegaray Ibañez1 y Francisco de la Cuesta Arzamendi1 del 1Hospital Donostia, Donostia-San Sebastián (Guipúzcoa) y 2Hospital de Galdakao (Vizcaya).
- 6018-559. Nuevo modelo murino de insuficiencia cardiaca. Optimización experimental
- Ana Giménez Pérez, Esther Roselló Lleti, Estefanía Tarazón Melguizo, Ana Ortega Gutiérrez, Micaela Molina Navarro, Manuel Portolés Sanz, Carlos Vila López y Miguel Rivera Otero del Hospital La Fe, Valencia.
- 6018-560. ¿Tiene la metformina un efecto positivo sobre la supervivencia en pacientes diabéticos con insuficiencia cardiaca con independencia del control glucémico?
- Clara Bonanad Lozano, Sergio García-Blas, Lourdes Bondanza Saavedra, Carla Valentina Castillo Soria, Silvia Ventura Haro, Juan Sanchís Forés, Francisco Javier Chorro Gascó y Julio Núñez Villota del Hospital Clínico Universitario, INCLIVA, Valencia.
- 6018-561. Evolución de la miocardiopatía dilatada alcohólica en función del nivel de ingesta de etanol
- Gonzalo Guzzo Merello, Pablo García-Pavía, Marta Cobo, Ana Briceño, María Dolores García-Cosío, Manuel Gómez-Bueno, Javier Segovia y Luis Alonso-Pulpón del Hospital Universitario Puerta de Hierro, Majadahonda (Madrid).
- 6018-562. Incidencia de arritmias letales y sus factores predictores en la miocardiopatía dilatada alcohólica
- Gonzalo Guzzo Merello, Pablo García-Pavía, Marta Cobo, Ana Briceño, Patricia Avellana, Manuel Gómez-Bueno, Javier Segovia y Luis Alonso-Pulpón del Hospital Universitario Puerta de Hierro, Majadahonda (Madrid).
- 6018-563. Estudio de la biología de los péptidos natriuréticos tisulares mediante RNAseq en pacientes con miocardiopatía dilatada
- Estefanía Tarazón Melguizo1, Ana Ortega Gutiérrez1, Esther Rosello Lleti1, Micaela Molina Navarro1, Plácido Orosa Martínez2, Begoña Igual Muñoz1, Miguel Rivera Otero1 y Manuel Portolés Sanz1 del 1Hospital La Fe, Valencia y 2Hospital de Gandía y Centro Especialidades Francesc de Borja, Gandía (Valencia).
- 6018-564. Alteraciones del proteoma mitocondrial en el tejido cardiaco de pacientes con miocardiopatía isquémica
- Esther Roselló Lleti, Estefanía Tarazón Melguizo, Ana Ortega Gutiérrez, Micaela Molina Navarro, Luis Martínez Dolz, Isabel Herrer Manbuena, Manuel Portolés Sanz y Miguel Rivera Otero del Hospital La Fe, Valencia.
- 6018-565. Influencia del tratamiento en la presentación de complicaciones neurológicas en la endocarditis infecciosa
- Elena Gómez Denia, Nuria Vallejo Camazón, María Luisa Pedro-Botet Montoya, Lourdes Mateu Pruñunosa, Raquel Núñez Aragón, Laia Llovera Rius y Antoni Bayes-Genis del Hospital Universitari Germans Trias i Pujol, Badalona (Barcelona).
- 6018-566. Perfil de los exitus tras terapia de resincronización cardiaca. Seguimiento a 9 años
- Rafaela del Carmen Ramírez Rodríguez1, Dámaso Valerón Hernández-Abad1, Antonia María Ramírez Rodríguez2, Miguel Ángel García Bello1, Antonio García Quintana1, José Ramón Ortega Trujillo1 y Alfonso Medina Fernández-Aceytuno1 del 1Hospital Universitario de Gran Canaria Dr. Negrín, Las Palmas de Gran Canaria y 2Hospital de Gran Canaria Insular Materno-Infantil, Las Palmas de Gran Canaria.
- 6018-567. Seguimiento a un año de pacientes con insuficiencia cardiaca: papel pronóstico de la monitorización ambulatoria de presión arterial
- Ana Mª González González1, Ana María García Bellón1, Beatriz Pérez Villardón1, M. Dolores Martínez Esteban2, Miguel Ángel Ramírez Marrero1, Pedro Aranda Lara2 y Manuel de Mora Martín1 del 1Servicio de Cardiología y 2Servicio de Nefrología, Hospital Regional Universitario Carlos Haya, Málaga.
- 6018-568. Alteraciones en la expresión de proteínas del ventrículo izquierdo de pacientes con cardiopatía isquémica
- Esther Roselló Lleti, Estefanía Tarazón Melguizo, Ana Ortega Gutiérrez, Micaela Molina Navarro, Luis Almenar Bonet, Antonio Salvador Sanz, Manuel Portolés Sanz y Miguel Rivera Otero del Hospital Universitario La Fe, Valencia.
- 6018-569. Expresión diferencial de los genes reguladores de los canales iónicos de cloro y potasio en miocardiopatía dilatada no isquémica
- Micaela Molina Navarro, Ana Ortega Gutiérrez, Estefanía Tarazón Melguizo, Esther Roselló Lleti, Isabel Herrer Mambrona, Ana Giménez Pérez, Manuel Portolés Sanz y Miguel Rivera Otero del Hospital Universitario La Fe, Valencia.
- 6018-570. Implementación de una unidad de insuficiencia cardiaca en un hospital no terciario
- Virgilio Martínez Mateo, José Plaza, María Eugenia Martín Barrios, Teresa Colchero Méniz, Miguel Ángel Villanueva, Ana Nieto y Antonio Paule del Complejo Hospitalario La Mancha Centro, Alcázar de San Juan (Ciudad Real).
- 6018-571. Importancia del especialista en la atención a la insuficiencia cardiaca descompensada. Resultados del estudio INCA
- Luciano Consuegra Sánchez1, Derek Dau1, Leticia Jaulent1, Francisco Javier Félix Redondo2, Luis Lozano Mera2, I. Miranda2, Yolanda Morcillo2 y Daniel Fernández Berges2 del 1Servicio de Cardiología, H.G.U. Santa Lucía, Cartagena (Murcia) y 2Unidad de Investigación Don Benito-Villanueva, Grupo GRIMEX, Fundesalud, Villanueva de la Serena (Badajoz).
- 6018-572. Magnitud de la disfunción sistólica ventricular izquierda grave y evolución del manejo terapéutico en nuestra área hospitalaria
- Ana Blanca Martínez, Ana López Suárez, Ana José Manovel, José Ignacio Morgado, María Teresa Moraleda, Agustín Tobaruela y José Francisco Díaz del Hospital Juan Ramón Jiménez, Huelva.
- 6018-573. Presentación clínica y perfil genético de las miocardiopatías familiares
- Carmen Jurado Canca, José Manuel García Pinilla, Miguel López Garrido, Juan Robledo Carmona, Eloy Rueda Calle, Fernando Cabrera Bueno, Juan José Gómez Doblas y Eduardo de Teresa Galván del Hospital Clínico Universitario Virgen de la Victoria, Málaga.
- 6018-574. Insuficiencia cardiaca refractaria en planta de cardiología
- María Lázaro Salvador, Fernando Álvaro López Sánchez, Ana M. García de Castro, Diana Segovia Herreras, Icíar García Ormazábal, Blanca Rodríguez Picón, Finn Olof Akerstrom y Luis Rodríguez Padial del Hospital Virgen de la Salud, Toledo.
- 6018-575. Disfunción auricular en la insuficiencia cardiaca con fracción de eyección preservada: papel en el inicio de los síntomas
- Laura Sanchís Ruiz1, Luigi Gabrielli1, Rut Andrea1, Carles Falces1, Nicolas Duchateau2, Félix Pérez-Villa1, Bart Bijnens2 y Marta Sitges1 del 1Servicio de Cardiología del Hospital Clínic, Barcelona y 2Hospital Clínic, Barcelona.
- 6018-576. Etiología e influencia sobre la mortalidad intrahospitalaria de la hipoalbuminemia en el paciente con insuficiencia cardiaca aguda
- Juan Luis Bonilla Palomas, Antonio Luis Gámez López, Mirian Moreno Conde, Cristina López Ibáñez, Ángel Gallego de la Sacristana López Serrano y Antonia Villar Ráez del Hospital San Juan de la Cruz, Úbeda (Jaén).
- 6018-577. La hipoalbuminemia detectada durante el ingreso predice la mortalidad a largo plazo del paciente hospitalizado por insuficiencia cardiaca aguda
- Juan Luis Bonilla Palomas, Antonio Luis Gámez López, Mirian Moreno Conde, Cristina López Ibáñez, Ángel Gallego de la Sacristana López Serrano y Antonia Villar Ráez del Hospital San Juan de la Cruz, Úbeda (Jaén).
- 6018-578. Cómo interpretar los resultados del TAPSE
- Ana García Martín, José Luis Moya Mur, Derly Becker Filho, Carlos Moreno Vinués, Eduardo Casas Rojo, Manuel Jiménez Mena, Covadonga Fernández Golfín y José Luis Zamorano Gómez del Hospital Universitario Ramón y Cajal, Madrid.
- 6018-579. Cambios anatomofuncionales del ventrículo derecho en pacientes obesos mórbidos tras cirugía bariátrica: estudio con resonancia magnética cardiaca
- Marcos Yacono1, María Luaces Méndez1, Jorge Cabezudo2, Victoria Cachofeiro3, Rosa Villar2, Ernesto Martínez3, Alejandro García Muñoz Najar2 y Leopoldo Pérez de Isla1 del 1Hospital Clínico San Carlos, Madrid, 2Hospital Universitario de Fuenlabrada, Madrid y 3Universidad Complutense, Madrid.
- 6018-580. Insuficiencia cardiaca crónica y fibrilación auricular: ¿es el déficit de hierro un nuevo factor etiológico?
- Cristina Enjuanes Grau, Andrés Fernández Gasalla, Begoña Benito Villabriga, Josep Comín Colet, Daniel Bueno López, Miguel Cainzos Achirica, Soledad Ascoeta Ortiz y Jordi Bruguera Cortada del Hospital del Mar, Barcelona.
- 6018-581. La normalización precoz de la función sistólica tras terapia de resincronización es mantenida a largo plazo e identifica a los pacientes con mejor pronóstico
- Fernando Cabrera Bueno, Amalio Ruiz Salas, Carmen Medina Palomo, José Peña Hernández, Julia Fernández Pastor, Alberto Barrera Cordero, Javier Alzueta y Eduardo de Teresa Galván del Hospital Clínico Universitario Virgen de la Victoria, Málaga.
- 6018-582. Pronóstico de la insuficiencia cardiaca de diagnóstico ambulatorio en nuestro medio: la fracción de eyección preservada tiene un pronóstico cardiovascular comparable a la reducida
- Rut Andrea Riba, Laura Sanchis Ruiz, Carlos Falces Salvador, Marta Sitges Carreño, Félix Pérez Villa, Magda Heras, Josep Brugada Terradellas y Manel Sabaté Tenas del Hospital Clínico, Barcelona.
- 6018-583. Aumento de la cardiotoxicidad de los esquemas de quimioterapia con antraciclinas que combinan trastuzumab
- José María Serrano Antolín1, Rosa M. Jiménez Hernández1, Silvia del Castillo Arrojo1, Iria A. González García1, Carmen Cristóbal Varela1, Luis Javier Morales García1, Javier Muñiz García2 y Joaquín J. Alonso Martín1 del 1Hospital Universitario de Fuenlabrada, Madrid y 2Instituto Universitario de Ciencias de la Salud, Universidad de A Coruña.
- 6018-584. Micropartículas de pequeño tamaño en la insuficiencia cardiaca sistólica. Posible implicación fisiológica en la respuesta isquémica
- Silvia Montoro García1, Diana Hernández-Romero1, Eva Jover1, Esteban Orenes-Piñero1, Antonio Tello-Montoliu1, Mariano Valdés-Chávarri1, Francisco Marín1 y Gregory Y.H. Lip2 del 1Departamento de Cardiología, Hospital Universitario Virgen de la Arrixaca, Cartagena, Murcia y 2City Hospital, Birmingham.
- 6018-585. Glucemia al ingreso y mortalidad a largo plazo en pacientes con insuficiencia cardiaca descompensada
- Antonio Luis Gámez López, Juan Luis Bonilla Palomas, María Cristina López Ibáñez, Mirian Moreno Conde, Ángel Gallego de la Sacristana López Serrano y Antonia Villar Ráez del Hospital San Juan de la Cruz, Úbeda (Jaén).
- 6018-586. Parámetros ecocardiográficos predictores de insuficiencia cardiaca derecha
- Ana García Martín, José Luis Moya Mur, Covadonga Fernández Golfín, Soledad Ruiz Leira, Alicia Megías Sáez, Miguel Castillo Orive, Mª Carmen de Pablo y Zarzosa y José Luis Zamorano Gómez del Hospital Universitario Ramón y Cajal, Madrid.
- 6018-587. Estudio farmacogenético de la ivabradina a través de identificación de los polimorfismos de los genes HCN4 y CYP3A4
- Manuel Hermida Prieto, Lucía Núñez, Eduardo Barge-Caballero, María Jesús Paniagua-Martín, Raquel Marzoa-Rivas, Zulaika Grille-Cancela, Alfonso Castro-Beiras y María G. Crespo-Leiro del Instituto de Investigación Biomédica A Coruña-INIBIC, Servicio de Cardiología-CHUAC, UDC, A Coruña.
- 6018-588. Factibilidad de la ultrafiltración lenta continua por vía periférica: ¿es posible en el mundo real?
- Nuria Ribas Barquet, Cristina Enjuanes Grau, Josep Comín Colet, Oona Meroño Dueñas, Cosme García García, Marcelo Rizzo, Luisa López Guillén y Jordi Bruguera Cortada del Hospital del Mar, Barcelona.
- 6018-589. Impacto pronóstico adverso a largo plazo de los valores de ácido úrico en pacientes hospitalizados por insuficiencia cardiaca aguda en un servicio de cardiología
- Cristina Victoria Iglesia Carreño1, Oscar Díaz Castro1, Inmaculada González Bermúdez2, Juan Ocampo Míguez1, Iñaki Villanueva Benito3, Itziar Solla Ruíz3, Sofía Vázquez Fernández4 y Andrés Iñiguez Romo1 del 1Hospital do Meixoeiro, Vigo (Pontevedra), 2Hospital POVISA, Vigo (Pontevedra), 3Hospital Donostia, Donostia-San Sebastián (Guipúzcoa) y 4Complejo Hospitalario de Pontevedra.
- 6018-590. Influencia de la presencia de diabetes en la valoración de la inervación cardiaca con gammagrafía con 123-metayodobencilguanidina en pacientes candidatos a implante de desfibrilador
- Pilar García González1, Puig Cozar Santiago2, Óscar Fabregat Andrés1, Raúl Sánchez Jurado2, Laura Higueras Ortega1, Andrés Cubillos Arango1, Joaquina Belchi Navarro1 y Francisco Ridocci Soriano1 del 1Consorcio Hospital General Universitario, Valencia y 2ERESA, Valencia.
- 6018-591. Programa de soporte circulatorio de corta duración con Levitronix Centrimag®. Impacto de un plan formativo en la curva de aprendizaje
- Marta Ruiz Lera1, Virginia Burgos Palacios1, Manuel Cobo Belaustegui1, Ángela Canteli Álvarez1, Cristina Castrillo Bustamante1, Miguel Llano Cardenal1, José Aurelio Sarralde Aguayo2 y José Maestre Alonso3 del 1Servicio de Cardiología del Hospital Universitario Marqués de Valdecilla, Santander (Cantabria), 2Servicio de Cirugía Cardiovascular del Hospital Universitario Marqués de Valdecilla, Santander (Cantabria) y 3Hospital Virtual Valdecilla, Santander (Cantabria).
- 6018-592. Papel de la ECMO venoarterial en el tromboembolismo pulmonar masivo: el comienzo de una nueva era
- Miguel Llano Cardenal, Ángela Canteli Álvarez, Cristina Castrillo Bustamante, Virginia Burgos Palacios, Marta Ruiz Lera, Manuel Cobo Belaustegui, Inmaculada García-Montesinos de la Peña y José Aurelio Sarralde Aguayo del Hospital Universitario Marqués de Valdecilla, Santander (Cantabria).
- 6018-592.1. MELD Scoring as a Predictor of Outcomes in Patients Presenting with Acute Decompensated Heart Failure
- Michael Scholfield, Matthew B. Schabath, Maya Guglin de la University of South Florida, Tampa, FL.
- 6018-593. Estudio de la rigidez hepática por elastografía (ARFI) en la insuficiencia cardiaca crónica descompensada
- Luis Caballero Jiménez, Carmen Muñoz Esparza, María Teresa Pérez Martínez, Francisco José Pastor Pérez, Iris Paula Garrido Bravo, Dolores Abellán Ribero, Manuel Reus Pintado y Domingo Pascual Figal del Hospital Clínico Universitario Virgen de la Arrixaca, Murcia.
- 6018-594. Impacto de un programa de dosis periódicas de levosimendán sobre la carga de arritmias ventriculares en pacientes con insuficiencia cardiaca avanzada
- Martín Jesús García González, Pablo Jorge Pérez, Julio Jesús Ferrer Hita, Aníbal Rodríguez González, Marco Giusseppe Cordero, Rubén Alfonso Juárez Prera, Esther González Cabeza e Ignacio Laynez-Cerdeña del Servicio de Cardiología, Hospital Universitario de Canarias, San Cristóbal de La Laguna (Santa Cruz de Tenerife).
- 6018-595. Mediciones seriadas del ancho de distribución eritrocitaria y su relación con el riesgo de desarrollo de anemia y muerte en pacientes con insuficiencia cardiaca
- Lourdes Bondanza Saavedra1, Julio Núñez Villota1, Gema Miñana Escrivá2, Carla Valentina Castillo Soria1, Sergio García Blas1, Clara Bonanad Lozano1, Francisco Javier Chorro Gascó1 y Juan Sanchís Forés1 del 1Hospital Clínico Universitario, Valencia y 2Hospital de Manises, Valencia.
- 6018-596. Mortalidad asociada al síncope en pacientes con insuficiencia cardiaca y relación con la presencia de función sistólica deprimida o preservada
- Domingo Andrés Pascual Figal1, Iris Garrido Bravo1, Juan Delgado Jiménez2, José Ramón González Juanatey3, Fernando Worner Diz4, Alfredo Bardají Ruiz5, Rafael Vázquez García6 y Juan Cinca Cuscullola7 del 1Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, 2Hospital Universitario 12 de Octubre, Madrid, 3Complexo Hospitalario Universitario de Santiago de Compostela, A Coruña, 4Hospital Universitari Arnau de Vilanova, Lérida, 5Hospital Universitario de Tarragona, 6Hospital Puerta del Mar, Cádiz y 7Hospital de la Santa Creu i Sant Pau, Barcelona.
- 6018-597. Control de frecuencia cardiaca en insuficiencia cardiaca. Frecuencia basal frente a media en registros prolongados
- Marina Navarro-Peñalver1, Francisco José Pastor Pérez1, Sergio Manzano-Fernández1, Rebeca Goya Esteban2, Domingo A. Pascual-Figal1, Óscar Barquero Pérez2, Mariano Valdés Chávarri1 y Arcadi García Alberola1 del 1Hospital Clínico Universitario Virgen de la Arrixaca, Murcia y 2Universidad Rey Juan Carlos, Madrid.
- 6018-598. Telemonitorización en pacientes con insuficiencia cardiaca: experiencia inicial con el sistema latitude
- Nahikari Salterain González, Alberto Esteban Fernández, Aitor Hernández Hernández, Manuel García de Yébenes Castro, Hugo Arguedas Jiménez, Naiara Calvo Galiano, Ignacio García Bolao y Juan José Gavira Gómez de la Clínica Universitaria de Navarra.
- 6018-599. El bortezomib, una alternativa eficaz en la amiloidosis cardiaca
- Inés Sayago Silva, Javier Segovia Cubero, Isabel Krsnik, Daniel Morillo, Manuel Gómez-Bueno y Luis Alonso-Pulpón del Hospital Universitario Puerta de Hierro, Madrid.
- 6018-600. Impacto de la conducción transeptal residual sobre la disincronía mecánica intraventricular izquierda en el bloqueo completo de rama izquierda
- Federico Ferrando Castagnetto1, Fabián Martínez Vergara1, Roberto Ricca Mallada1, Rodolfo Ferrando Castagnetto2, Alejandro Vidal Margenat1, Diego Freire Colla1, Álvaro Rivara Capocasale1 y Ricardo Lluberas Jabif1 del 1Departamento de Cardiología, Hospital de Clínicas, Montevideo y 2Servicio de Medicina Nuclear, Centro Asistencial del Sindicato Médico del Uruguay, Montevideo.
- 6018-601. Remodelado inverso del ventrículo izquierdo en pacientes con insuficiencia cardiaca y fracción de eyección deprimida: efecto del tratamiento médico
- Eduardo Barge Caballero, Sergio Chávez Leal, Rolando Joel Álvarez, Raquel Marzoa Rivas, María Jesús Paniagua-Martín, Fernando García López, Alfonso Castro Beiras y Marisa Crespo Leiro del CHUAC, A Coruña.
- 6018-602. Detección de cardiotoxicidad precoz mediante técnicas de strain longitudinal y su relación con el desarrollo de eventos clínicos
- Sandra Ofelia Rosillo Rodríguez, Silvia Cayetana Valbuena López, Teresa López Fernández, Ángel Manuel Iniesta Manjavacas, Gemma Daniele, Susana del Prado Díaz, M. del Mar Moreno Yangüela y José Luis López Sendón del Hospital Universitario La Paz, Madrid.
- 6018-603. Valor pronóstico del estudio ecocardiográfico y los dispositivos de asistencia ventricular en las miocarditis fulminantes
- Sandra Secades González, Cecilia Corros Vicente, María Martín Fernández, Jesús Mª de la Hera Galarza, Elena Díaz Peláez, Eloy Fernández García, Esmeralda Capín Sampedro y José Luis Lambert Rodríguez del Hospital Universitario Central de Asturias, Oviedo (Asturias).
