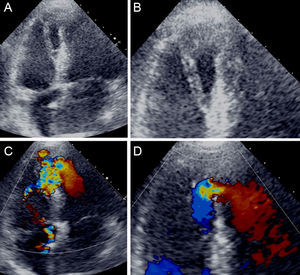
An 81-year-old chronically hypertensive woman presented to our emergency department with a 4-day history of crescendo angina pectoris with associated nausea and vomiting. On admission she was anxious, hypotensive (94/68mmHg), tachycardic (119 bpm) and had a loud holosystolic murmur, III/VI, best heard at the lower sternal border with no signs of pulmonary or peripheral congestion. The electrocardiogram showed sinus tachycardia (121 bpm), a QS pattern at leads V1-V2, and nonspecific repolarization abnormalities. Blood analysis revealed mildly elevated troponin T (1.3 ng/mL). After being admitted to the coronary unit, the patient underwent a transthoracic echocardiogram revealing akinesis of the apex and middle/distal interventricular septum with a large interventricular dissection and apical septum defect, through which a significant left-to-right shunt with a Qp/Qs of 2.6 and a pressure gradient of 40mmHg could be observed (Figures A-D and ). The coronary angiogram showed a total occlusion of the distal left anterior descending artery.
The patient remained relatively stable and 3 weeks after admission underwent successful corrective surgery of the interventricular septum defect with a bovine pericardial patch. She had an uneventful postoperative period, experiencing only mild cognitive impairment. She is now doing well after a prolonged period of recovery in a long-term care unit.
Dissection of the interventricular septum is a rare complication of acute myocardial infarction, most commonly associated with inferior wall infarcts. It is considered a subacute form of cardiac rupture, resulting from intramural hematoma formation and propagation between the spiral myocardial fibres.