We report the case of a 47-year-old man with end-stage ischemic heart disease who underwent implantation of a Berlin Heart EXCOR® biventricular assist device (VAD) as a bridge to transplantation (Figure 1). He received oral anticoagulation and dual antiplatelet therapy with acetylsalicylic acid and clopidogrel, according to the standard protocol until, 1 month later, he had a hemorrhagic stroke that left no sequelae. Therefore, the decision was made to discontinue the antiplatelet therapy and to treat the patient with acenocoumarol alone.
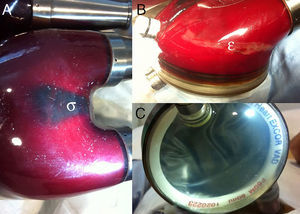
Three months later, he came to the emergency service because of a warning from the VAD that indicated low flow in the system. He had an international normalized ratio (INR) of 2.6. Inspection of the left VAD (Figures 2A and 2B and video clip [supplementary material]) revealed a moving shadow (σ) associated with a thrombus that grew rapidly (¿) within the blood chamber, in addition to an abnormal expansion of the outer membrane during systole (Figure 2C). As we suspected rupture of 1 of the membranes that separate the 2 chambers (blood and air) and because of the risk of systemic embolization of the thrombus, the left VAD cannulas were rapidly clamped and the flow in the right VAD was reduced to prevent acute pulmonary edema. The malfunctioning VAD was replaced, (Figure 3) and rupture of the inner membrane (*) of the explanted device and the presence of a large associated thrombus (δ) were confirmed. The outcome of this replacement was favorable and the patient received a transplant several weeks later.
Thrombotic complications associated with VAD are relatively frequent and potentially fatal events. In this case, early identification of the problem and urgent intervention allowed successful replacement of the device and subsequent transplantation.