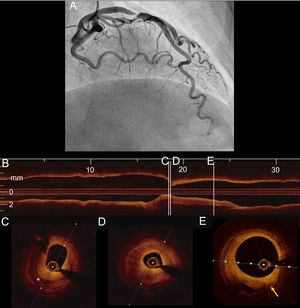
A hypertensive 59-year-old woman was admitted for an episode of chest pain at rest. The electrocardiogram was normal, but a rise in troponin I was detected. Coronary angiography revealed a severe focal stenosis in the proximal segment of the left anterior descending artery (Figure 1A), without any other stenosis in the coronary tree. Optical coherence tomography was performed to clarify the substrate of the stenosis. The coronary lumen was narrowed (Figure 1B, 1C, and 1D) by an atherosclerotic plaque with a heterogeneous structure, with a low-reflectivity half-moon shaped region that contrasted with the surrounding fibrous tissue (asterisk in Figure 1C). No disruption of the intima or luminal thrombus was observed. Microvessels (Figure 1E: arrow) were visible in the vicinity of the plaque and in connection with the above-mentioned half-moon shaped region, suggesting that the low reflectivity noted in that structure could be the result of intraplaque hemorrhage. The lesion was treated with a drug-eluting stent with good outcome. Intraplaque hemorrhage, resulting from leaky plaque neovascularization, has been described as a mechanism for rapid plaque growth and instability and could have been the cause of acute coronary syndrome in our patient. Optical coherence tomography was useful to clarify the stenosis substrate and exclude other causes of acute coronary syndrome in young women, such as spontaneous coronary dissection and coronary erosion. This imaging technique is also able to differentiate intraplaque hemorrhage (occurring within an atherosclerotic plaque located in the intima) from an intramural haematoma, ie a separation of the intima and media from the adventitia generally found in nonatherosclerotic arteries.
Conflicts of InterestN. Gonzalo has received speaker honoraria for educational activities from Abbot.