To analyze the clinical impact of the inappropriate use of antithrombotic treatment in patients with high ischemic or hemorrhagic risk during the periprocedural/perisurgical period in Spain.
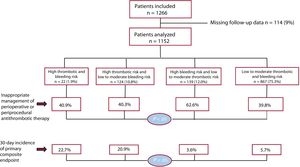
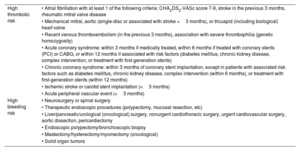
MethodsProspective multicenter observational registry of patients receiving antiplatelet and/or anticoagulant therapy who required an intervention. The incidence of 30-day events was compared based on the peri-intervention management of antithrombotic treatment and the patients’ risk classification (high vs. moderate-to-low risk). The primary endpoint was a composite of death, cardiovascular ischemic events, or bleeding events classified as BARC 2 or higher.
ResultsA total of 1152 patients were analyzed. Of these, 1.9% had both high ischemic and hemorrhagic risks (A);10.8% had high ischemic risk and low-to-moderate hemorrhagic risk (B); 12% had high hemorrhagic risk and low-to-moderate ischemic risk (C); and 75.3% had both low-to-moderate risks (D). The prevalence of inappropriate treatment was higher in the subgroup with high hemorrhagic risk and low-to-moderate ischemic risk (C) (62.6% vs 40.9% in subgroup A; P<.05; 40.3% in subgroup B; P<.001; and 39.8% in subgroup D; P<.05). The incidence of the composite endpoint was higher in the subgroups with high ischemic and hemorrhagic risks (22.7%) and high ischemic and low-to-moderate hemorrhagic risks (20.9%), compared with 3.6% in subgroup C (P<.05) and 5.7% in subgroup D (P<.001). Among patients with inappropriate treatment, the incidence of the composite endpoint was significantly higher in subgroups with high ischemic and hemorrhagic risks (44.4% vs 7.7%; P=.043) and high ischemic and low-to-moderate hemorrhagic risks (30% vs 14.8%; P=.042).
ConclusionsThe prevalence of inappropriate periprocedural/perisurgical treatment was higher in patients with high hemorrhagic risk and low-to-moderate ischemic risk. The incidence of events was higher in patients with high ischemic risk, with inadequate antithrombotic management being associated with a higher event rate in these groups.
Keywords
Identify yourself
Not yet a subscriber to the journal?
Purchase access to the article
By purchasing the article, the PDF of the same can be downloaded
Price: 19,34 €
Phone for incidents
Monday to Friday from 9am to 6pm (GMT+1) except for the months of July and August, which will be from 9am to 3pm