The clinical profile of arrhythmogenic cardiomyopathy (ACM) with left ventricular (LV) involvement appears to be distinct from ACM isolated to the right ventricle (RV)1,2, with a higher incidence of ventricular arrhythmias and sudden cardiac death (SCD) shown in some studies.3 However, in Spain, there are few published series correlating LV involvement with an increased risk of arrhythmia and SCD.
Our aim was to analyze the differentiating clinical and morphological characteristics of biventricular ACM compared with ACM isolated to the RV in our series. This was a cross-sectional study that included 30 patients with ACM from 20 families; 17 were probands (56.7%) and 13 were relatives. All met the Task Force criteria for ACM. Participants were divided into 2 groups according to whether they had involvement of the RV alone or biventricular involvement (the LV was considered involved when the ejection fraction on echocardiography was < 50%).
Data were collected on age and sex, as well as clinical information on functional class, syncope, ventricular arrhythmias, atrial fibrillation, implantable cardioverter-defibrillator (ICD) shocks, heart transplantation, and death due to end-stage heart failure. All participants were studied with 12-lead ECG, echocardiography, and where possible, cardiac magnetic resonance (MR). Genetic study was performed in 27 patients (90%).
The statistical analysis was performed by comparing these variables in relation to the presence of isolated RV involvement or biventricular involvement, and nonparametric tests (Mann-Whitney U test) were used for the study of the mean.
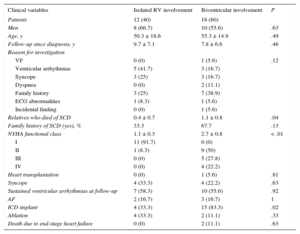
Biventricular involvement was predominant in the probands and relatives. Of a total of 55 relatives studied, 18.2% received a new diagnosis of ACM. Follow-up time from diagnosis was similar in both groups (Table 1). In addition, in the group with biventricular involvement, 89% of the patients already had LV involvement at the time of diagnosis. No significant differences were found in the presence of epsilon waves and bundle branch block on ECG, but there was a trend (P = .07) toward an increased presence of inverted T waves in the precordial leads in the group with biventricular involvement.
Statistical Comparison of Baseline Clinical Variables Between the Groups With Isolated RV Involvement and Biventricular Involvement
| Clinical variables | Isolated RV involvement | Biventricular involvement | P |
|---|---|---|---|
| Patients | 12 (40) | 18 (60) | |
| Men | 8 (66.7) | 10 (55.6) | .63 |
| Age, y | 50.3 ± 18.6 | 55.3 ± 14.9 | .49 |
| Follow-up since diagnosis, y | 9.7 ± 7.1 | 7.8 ± 6.6 | .46 |
| Reason for investigation | |||
| VF | 0 (0) | 1 (5.6) | .12 |
| Ventricular arrhythmias | 5 (41.7) | 3 (16.7) | |
| Syncope | 3 (25) | 3 (16.7) | |
| Dyspnea | 0 (0) | 2 (11.1) | |
| Family history | 3 (25) | 7 (38.9) | |
| ECG abnormalities | 1 (8.3) | 1 (5.6) | |
| Incidental finding | 0 (0) | 1 (5.6) | |
| Relatives who died of SCD | 0.4 ± 0.7 | 1.1 ± 0.8 | .04 |
| Family history of SCD (yes), % | 33.3 | 67.7 | .13 |
| NYHA functional class | 1.1 ± 0.3 | 2.7 ± 0.8 | < .01 |
| I | 11 (91.7) | 0 (0) | |
| II | 1 (8.3) | 9 (50) | |
| III | 0 (0) | 5 (27.8) | |
| IV | 0 (0) | 4 (22.2) | |
| Heart transplantation | 0 (0) | 1 (5.6) | .81 |
| Syncope | 4 (33.3) | 4 (22.2) | .63 |
| Sustained ventricular arrhythmias at follow-up | 7 (58.3) | 10 (55.6) | .92 |
| AF | 2 (16.7) | 3 (16.7) | 1 |
| ICD implant | 4 (33.3) | 15 (83.3) | .02 |
| Ablation | 4 (33.3) | 2 (11.1) | .33 |
| Death due to end-stage heart failure | 0 (0) | 2 (11.1) | .63 |
AF, atrial fibrillation; ECG, electrocardiogram; ICD, implantable cardioverter-defibrillator; NYHA, New York Heart Association; RV, right ventricle; SCD, sudden cardiac death; VF, ventricular fibrillation.
Unless otherwise stated, values are expressed as no. (%) or mean ± standard deviation.
Table 1 shows the clinical characteristics of the groups with isolated RV involvement and with biventricular involvement. The functional class was clearly more advanced in the biventricular group. Although the presence of syncope and ventricular arrhythmias was similar, the burden of family history of SCD was higher in patients with biventricular involvement (P = .04). However, on dichotomous analysis (yes/no) of this family history, a trend was found; this did not reach statistical significance (P = .13). More ICDs were implanted in the biventricular group, mainly as primary prevention (66.7% of implants); none of the patients with isolated RV involvement received an ICD for this indication. The distribution of ICD therapies differed according to the indication (P < .01): there was a higher number of appropriate shocks in the group with an ICD as secondary prevention (88.9%), while a minority of the patients with an ICD as primary prevention had received appropriate ICD therapies at follow-up (10%). These findings were similar to those observed in other registries.4
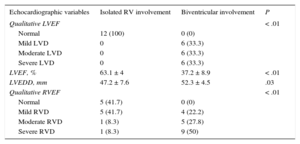
Investigation of ventricular function showed an increased LV end-diastolic diameter and a higher degree of RV and LV dysfunction in patients with biventricular involvement (Table 2). A limitation of this study is the insufficient availability of additional data from MR.
Statistical Comparison of Echocardiographic Data Between the Groups With Isolated RV Involvement and Biventricular Involvement
| Echocardiographic variables | Isolated RV involvement | Biventricular involvement | P |
|---|---|---|---|
| Qualitative LVEF | < .01 | ||
| Normal | 12 (100) | 0 (0) | |
| Mild LVD | 0 | 6 (33.3) | |
| Moderate LVD | 0 | 6 (33.3) | |
| Severe LVD | 0 | 6 (33.3) | |
| LVEF, % | 63.1 ± 4 | 37.2 ± 8.9 | < .01 |
| LVEDD, mm | 47.2 ± 7.6 | 52.3 ± 4.5 | .03 |
| Qualitative RVEF | < .01 | ||
| Normal | 5 (41.7) | 0 (0) | |
| Mild RVD | 5 (41.7) | 4 (22.2) | |
| Moderate RVD | 1 (8.3) | 5 (27.8) | |
| Severe RVD | 1 (8.3) | 9 (50) |
LVD, left ventricular dysfunction; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; RV, right ventricle; RVD, right ventricular dysfunction; RVEF, right ventricular ejection fraction.
Unless otherwise stated, values are expressed as no. (%) or mean ± standard deviation.
The results confirm that biventricular involvement represents a more advanced stage of isolated RV disease. Our study corroborates the association between LV involvement and a more advanced functional class. Certainly, previous studies have established the relationship between LV involvement and an increased mortality rate due to heart failure.1,5,6 However, although the analysis of our series does not demonstrate a significant association, it does shows a trend: the 2 patients who died from heart failure and the single patient who received a transplant were all from the biventricular involvement group. The lack of significance is probably due to an insufficient sample size. Regarding the risk of arrhythmia, of the group with isolated RV involvement, 4 patients had ICDs as secondary prevention compared with only 2 in the biventricular group. In contrast, all ICDs implanted as primary prevention were in patients with biventricular involvement, because their risk profile was higher based on the presence of significant LV dysfunction3 (Table 1). These differences could explain why the incidence of arrhythmic events was similar in both groups at follow-up, even though a relationship with the presence of LV dysfunction would have been expected.
We can conclude that LV dysfunction is associated with greater RV dysfunction, worse functional class, and an increased tendency to events due to heart failure. No clear relationship was found between LV involvement and an increased rate of arrhythmic events, although there was an association with an increased burden of family history of SCD.