Mechanical complications (MC) of ST-segment-elevation acute myocardial infarction (STEMI) are an important cause of morbidity and mortality and dramatically worsen prognosis. The introduction of early reperfusion therapy has significantly reduced the classical incidence of MC (5%-10%).1,2 In particular, the widespread use of primary angioplasty (PA) has reduced its current incidence to between 1% and 2%.3,4 The implementation of regional PA programs has decreased reperfusion times and improved prognosis, most likely due to the decreased incidence of MC. We evaluated the incidence, treatment, course, and predictors of MC in a cohort who underwent PA under a STEMI emergency treatment protocol, in which fibrinolysis was only used when there were delays or logistic difficulties.
Four researchers retrospectively reviewed the medical records of 950 consecutive patients who underwent PA between 2005 and 2012 with hospital and 30-day follow-up. Qualitative variables are expressed as percentages and quantitative variables as mean or median ± standard deviation according to the normality of the distribution. The Student t test was used to compare means and chi-square for percentages. Univariable and multivariable analyses were used to identify the predictors of MC. A P value of < .05 was used as a cutoff for statistical significance.
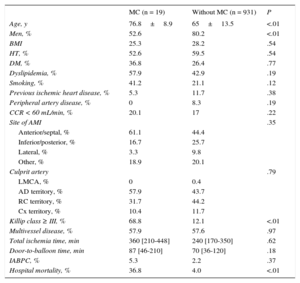
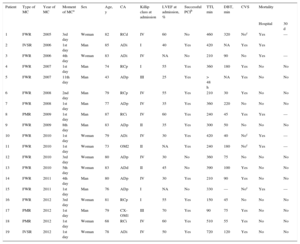
The incidence of MC was 2.02% (19 patients). Of these patients, 14 (73.6%) had free wall rupture (FWR), 2 (10.5%) had interventricular septal rupture (IVSR), and 3 (15.8%) had papillary muscle rupture (PMR). Most MCs occurred within 24hours of admission (52.6%) and a significant proportion (26.3%) occurred after 96hours. Table 1 shows the baseline characteristics of the patients and Table 2 shows the characteristics of the patients with MCs. The median total times of ischemia (symptoms-to-balloon) and door-to-balloon were nonsignificantly higher in the MC group. Regarding treatment and in-hospital course, 7 patients died (36.8%) and 10 patients (52.6%) were referred to cardiac surgery. One patient died before surgery, but the remaining 9 patients survived. All patients with PMR or IVSR underwent surgery, whereas 5 (35.7%) of the patients with FWR underwent surgery and 5 with FWR (35.7%) underwent intensive medical treatment. Patients with IVSR did not undergo percutaneous treatment due to its lack of availability. These treatment options were not applicable in the remaining patients with FWR (28.6%), because of sudden death. Logistic regression analysis showed that the only independent predictors of events were female sex (odds ratio [OR] = 4.03; confidence interval 95% [95%CI], 1.2-14.9; P = .022) and Killip class III-IV (OR = 1.95; 95%CI, 1.9-4.5; P < .0001).
Baseline Characteristics of Patients With and Without Mechanical Complications and Their Comparison
| MC (n = 19) | Without MC (n = 931) | P | |
|---|---|---|---|
| Age, y | 76.8±8.9 | 65±13.5 | <.01 |
| Men, % | 52.6 | 80.2 | <.01 |
| BMI | 25.3 | 28.2 | .54 |
| HT, % | 52.6 | 59.5 | .54 |
| DM, % | 36.8 | 26.4 | .77 |
| Dyslipidemia, % | 57.9 | 42.9 | .19 |
| Smoking, % | 41.2 | 21.1 | .12 |
| Previous ischemic heart disease, % | 5.3 | 11.7 | .38 |
| Peripheral artery disease, % | 0 | 8.3 | .19 |
| CCR < 60 mL/min, % | 20.1 | 17 | .22 |
| Site of AMI | .35 | ||
| Anterior/septal, % | 61.1 | 44.4 | |
| Inferior/posterior, % | 16.7 | 25.7 | |
| Lateral, % | 3.3 | 9.8 | |
| Other, % | 18.9 | 20.1 | |
| Culprit artery | .79 | ||
| LMCA, % | 0 | 0.4 | |
| AD territory, % | 57.9 | 43.7 | |
| RC territory, % | 31.7 | 44.2 | |
| Cx territory, % | 10.4 | 11.7 | |
| Killip class ≥ III, % | 68.8 | 12.1 | <.01 |
| Multivessel disease, % | 57.9 | 57.6 | .97 |
| Total ischemia time, min | 360 [210-448] | 240 [170-350] | .62 |
| Door-to-balloon time, min | 87 [46-210] | 70 [36-120] | .18 |
| IABPC, % | 5.3 | 2.2 | .37 |
| Hospital mortality, % | 36.8 | 4.0 | <.01 |
AD, anterior descending; AMI, acute myocardial infarction; BMI, body mass index; CCR, creatinine clearance rate; Cx, circumflex; DM, diabetes mellitus; HT, hypertension; IABCP, intra-aortic balloon counter pulsation; LMCA, left main coronary artery; MC, mechanical complication; RC, right coronary.
Unless otherwise specified, values are expressed as mean ± standard deviation or median [interquartile range].
Characteristics of Patients With Mechanical Complications
| Patient | Type of MC | Year of MC | Moment of MCa | Sex | Age, y | CA | Killip class at admission | LVEF at admission, % | Successful PCIb | TTI, min | DBT, min | CVS | Mortality | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital | 30 d | |||||||||||||
| 1 | FWR | 2005 | 3rd day | Woman | 82 | RCd | IV | 60 | No | 460 | 320 | Noc | Yes | — |
| 2 | IVSR | 2006 | 1st day | Man | 85 | ADi | I | 40 | Yes | 420 | NA | Yes | Yes | |
| 3 | FWR | 2006 | 4th day | Woman | 83 | ADi | IV | NA | No | 210 | 90 | No | Yes | — |
| 4 | FWR | 2007 | 1st day | Man | 74 | RCp | I | 55 | Yes | 360 | 180 | Yes | No | No |
| 5 | FWR | 2007 | 11th day | Man | 43 | ADp | III | 25 | Yes | > 48 h | NA | Yes | No | No |
| 6 | FWR | 2008 | 2nd day | Man | 79 | RCp | IV | 55 | Yes | 210 | 30 | Yes | No | No |
| 7 | FWR | 2008 | 1st day | Man | 77 | ADp | IV | 35 | Yes | 360 | 220 | No | No | No |
| 8 | PMR | 2009 | 1st day | Man | 87 | RCi | IV | 60 | Yes | 240 | 45 | Yes | Yes | — |
| 9 | FWR | 2009 | 8th day | Man | 83 | ADp | II | 35 | Yes | 300 | 50 | No | No | No |
| 10 | FWR | 2010 | 1st day | Woman | 79 | ADi | IV | 30 | Yes | 420 | 40 | Noc | Yes | — |
| 11 | FWR | 2010 | 1st day | Woman | 73 | OM2 | II | NA | Yes | 240 | 180 | Noc | Yes | — |
| 12 | FWR | 2010 | 3rd day | Woman | 80 | ADp | IV | 30 | No | 360 | 75 | No | No | No |
| 13 | FWR | 2010 | 5th day | Woman | 83 | ADd | II | 45 | No | 390 | 100 | Yes | No | No |
| 14 | FWR | 2011 | 4th day | Man | 80 | ADp | IV | 30 | Yes | 210 | 90 | Yes | No | No |
| 15 | FWR | 2011 | 1st day | Man | 76 | ADp | I | NA | No | 330 | — | Noc | Yes | — |
| 16 | FWR | 2012 | 3rd day | Woman | 81 | RCp | I | 55 | Yes | 150 | 45 | No | No | No |
| 17 | PMR | 2012 | 1st day | Man | 79 | CX-OM1 | III | 70 | Yes | 90 | 75 | Yes | No | No |
| 18 | PMR | 2012 | 1st day | Woman | 68 | RCi | IV | 60 | Yes | 510 | 55 | Yes | No | No |
| 19 | IVSR | 2012 | 1st day | Woman | 78 | ADi | IV | 50 | Yes | 720 | 120 | Yes | No | No |
AD, anterior descending; CA, culprit artery; CVS, cardiovascular surgery; CX-OM1, circumflex-first marginal; d, distal; DBT, door-to-balloon time; FWR, free wall rupture; i, intermediate; IVSR, interventricular septal rupture; LVEF, left ventricular ejection fraction; MC, mechanical complication; NA, not available; OM2, second marginal; p, proximal; PCI, percutaneous coronary intervention; PMR, papillary muscle rupture; RC, right coronary; TIMI, Thrombolysis in Myocardial Infarction; TTI, total time of ischemia.
The incidence of MC was similar to that described in the literature1,2, but clearly lower than its incidence (5%-10%) in the period before widespread implementation of systematic reperfusion. Some characteristics have already been described as predictors of MC: female sex and longer ischemia times.4 In our series, Killip class III-IV was also an independent predictor of MC.
Current guidelines5 recommend surgery as the treatment of choice; however, some patients are not candidates for emergency surgery because of instability, age, and comorbidity. In addition, the optimal timing of surgical treatment remains to be established. Surgical mortality in these patients is considerable and is clearly influenced by those who survive the first days of stabilization under intensive measures, which constitutes a selection bias in most of the reported results. In our series, 52.6% of patients were referred to surgery, and around half of the patients with FWR received intensive medical treatment with acceptable results. Most of these patients had subacute FWR, which successfully responds to nonsurgical treatment.6
Regardless of treatment, prognosis is clearly worse in these patients and depends on the type of MC. In a series published by French et al.,4 in-hospital survival and 90-day survival were 97% and 96% in patients without MC, respectively. However, in-hospital survival and 90-day survival were 43% and 27% in patients with FWR, 73% and 73% in those with PMR, and 60% and 20% in those with IVSR, respectively. Overall 30-day survival was 63.2%, which varied according to the type of MC: 64.3% in FWR, 66.6% in PMR, and 50% in IVSR.
In conclusion, the incidence of MC has decreased in the era of PA, but remains associated with high mortality; however, the mortality rate could decrease in a group selected for surgery. Early diagnosis and treatment would be improved by remaining alert to the specific characteristics of each patient. The incidence of MC could be reduced by the widespread use of PA protocols with shorter ischemia times. Multicenter registries with more patients are needed to better understand the predictors of MC and to determine which subgroups would derive the most benefit from surgical treatment.