A 29-year-old man under treatment for 3 years with valsartan, amlodipine, and bisoprolol for hypertension and with no other relevant history sought medical attention for atypical chest pain and palpitations. Ischemic heart disease was ruled out and cardiac magnetic resonance (CMR) and blood tests were requested due to suspected secondary hypertension.
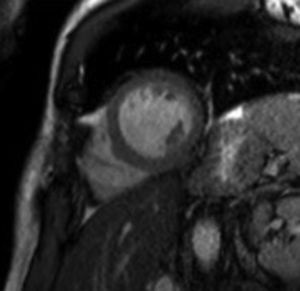
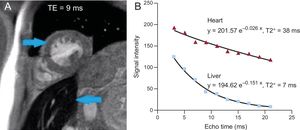
Microalbuminuria was detected (208mg/L). CMR showed eccentric left ventricular hypertrophy (weight, 198g) (Figure 1), normal systolic function, and reduced distensibility of the ascending aorta (2.3 × 10–3 mmHg–1). Coarctation of the aorta was ruled out. The adrenal glands and kidneys appeared to be normal (Figure 2). There was low signal intensity in the liver in multislice sequences. Multiecho sequences with increasing echo times (TEs) were acquired to calculate the T2* time constant (Figure 3A, the blue arrow on the left indicates the myocardium; the blue arrow on the right indicates the liver). A markedly decreased T2* of 7ms was obtained for the liver, indicating severe iron overload. There was no iron overload in the myocardium (T2* = 38ms) (Figure 3B). Blood testing confirmed the presence of C282Y homozygous hemochromatosis. The patient was treated with bloodletting until the normalization of serum ferritin levels. At 6 months, the patient's blood pressure was controlled with olmesartan monotherapy. Follow-up CMR showed reduced ventricular mass (weight, 175g) and very slight increased aortic distensibility (2.61 × 10–3 mmHg–1).
Hemochromatosis-related hypertension is associated with polycythemia, increased aortic wall stiffness, and the development of metabolic syndrome. Periodic bloodletting permits normalization of ferritin concentrations and helps to control blood pressure.
In CMR studies, it is essential to review the structures surrounding the heart to detect incidental findings of potential clinical interest.