Coronary lithoplasty is a novel treatment that uses high-energy mechanical pulses to break up calcium deposits in atherosclerotic heart disease. These pulses, known as shockwaves, are also used to break up calcium in other locations, especially the kidneys (lithotripsy). Their use in the heart is very new and there have been very few reported cases.1,2
Coronary lithoplasty involves the use of a nylon ball that, once positioned at the target site, is connected to an external unit that generates pulsatile mechanical waves lasting microseconds. The pulses are emitted on demand and deliver an intermittent pressure of 50 to 60atm to the vessel wall. This pressure is 3 to 4 times higher than that achieved using other devices. Balloon size must be such to achieve a balloon to artery ratio of 1:1, as the mechanical energy is generated and transmitted along the vessel wall when the balloon makes contact with the arterial intima.1 As the waves travel along the wall and through the connective tissue, they cause microfractures in the calcified tissues, allowing good lesion expansion and correct stent placement.2
We present the cases of 3 patients with multivessel coronary artery disease in whom 6 severely calcified lesions were successfully treated with coronary lithoplasty. The 3 patients all had characteristics that typically call for interventional treatment: advanced age and functional class, high surgical risk, previous revascularization, and a high probability of rotational atherectomy.
The lithoplasty balloon was successfully used to treat all 6 lesions and there were no intraprocedural complications, such as dissections or perforations.
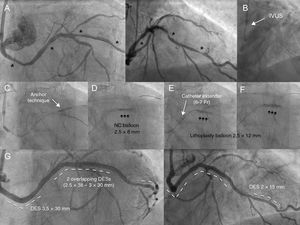
The first patient was a 73-year-old man with severe kidney failure who had undergone bilateral iliofemoral bypass. He had triple-vessel heart disease. Of note, the circumflex artery (Cx) arose in the right sinus and had 3 features that contraindicated percutaneous treatment: calcification, severe tortuosity, and diffuse distal disease (Figure 1A, ). The left anterior descending artery (LAD) was treated first, using coronary lithoplasty followed by drug-eluting stent (DES) placement. The Cx was treated in the same procedure using a multipurpose catheter and 2 guide catheters. Following unsuccessful advancement of the catheter via intravascular ultrasound (Figure 1B) and failure to successfully apply the side-branch anchor technique (Figure 1C), the medial lesion was partially dilated with a 2.5-mm noncompliant balloon (Figure 1D) (). This maneuver allowed us to advance the catheter extender (6-7 Fr) and correctly position the 2.5-mm lithoplasty balloon; the lesion was successfully expanded with 60 pulses (Figure 1E-F). The proximal and medial lesions were treated with a 3-mm lithoplasty balloon and placement of 4 DES (Figure 1G and ).
A: Calcified, tortuous circumflex artery with distal, medial, and proximal lesions (asterisks). B: The intravascular ultrasound (IVUS) catheter could not be advanced. C: Application of the side-branch anchor technique did not allow advancement of the lithoplasty balloon. D: Underexpansion of the 2.5-mm noncompliant (NC) balloon in the medial area helped advance the catheter extender and move the lithoplasty balloon forward (E). E: Unsuccessful dilation with 40 pulses. F: Opening of lesion after 60 pulses. G: Outcome after placement of 4 drug-eluting stents (DES).
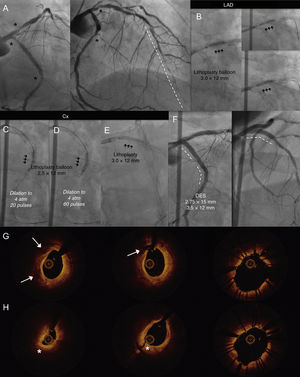
The second patient was a 63-year-old diabetic man with triple-vessel disease. Surgical revascularization had not been possible in 2014 because of the poor condition of the distal bed of the LAD. The patient's condition was initially treated with rotational atherectomy applied to the dominant CX and placement of 3 DESs. In 2018, a coronary angiogram performed to investigate refractory angina showed calcified lesions in the Cx (an ostial lesion and a lesion distal to the stent) and the LAD (an ostial lesion) (Figure 2A and ). The 3 lesions were treated with coronary lithoplasty (Figure 2B-E) and the results were excellent (Figure 2F and ). Optical coherence tomography showed several fracture points in the intimal and even the medial plaque (Figure 2G and H).
A: Calcified lesions in the ostial and medial-distal circumflex artery (Cx) and ostial left anterior descending artery (LAD) (asterisks) with diffuse disease in the distal LAD (dotted line). Coronary lithoplasty with a 3-mm balloon in the ostial DA (B) and the medial-distal Cx. Dilation to 4 atm and delivery of 20 pulses (C) and 60 pulses (D). E: Coronary lithoplasty with a 3-mm balloon in the ostial LAD. F: Placement of 3 drug-eluting stents, with good results; optical coherence tomography images before coronary lithoplasty; fracture of calcified plaque (arrows) and dissection of fibrous plaque (asterisks). G and H: Images after coronary lithoplasty and placement of stent in the ostial (G) and medial-distal Cx (H).
The third patient was an 81-year-old woman with heart disease not amenable to surgical treatment due to distal disease. In an initial step, the proximal right coronary artery was treated with rotational atherectomy. The distal truncus arteriosus and the proximal-medial LAD were both treated in a subsequent step (). The distal LAD was treated with a noncompliant balloon and a 2-mm cutting balloon. The proximal LAD and distal truncus arteriosus were treated with coronary lithoplasty and 2 overlapping DESs. The distal truncus arteriosus required postdilation with a double-layered balloon ().
Based on our preliminary experience, coronary lithoplasty is a) a safe and effective procedure for cases in which rotational atherectomy is not an option; b) a simple procedure with no learning curve that can be performed using standard guide catheters, and c) a procedure that permits protection of the lateral branches. The current balloon profile, however, is lower than that of state-of-the-art noncompliant balloons and needs to be improved, as it requires a catheter of at least 6 Fr. Lithoplasty balloons are currently available in just one length (12 mm) and have a diameter ranging from 2.5 to 4 mm.
In conclusion, coronary lithoplasty is a safe and effective procedure for treating severely calcified coronary lesions and will probably become an important addition to the armamentarium for modifying calcified plaque.3
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2018.11.017.