Keywords
INTRODUCTION
The pressure-guidewire is a valuable instrument for assessing the ischemic significance of coronary lesions, and is widely used in catheterization laboratories nowadays.1 This success is based on the measurement of a powerful determining index, the fractional flow reserve (FFR). The precise cut-off value (<0.75) of this index discriminates between lesions with and without ischemic potential.2 FFR allows the interventional cardiologist to direct his management strategy of intermediate lesions. In those cases with a FFR>=0.75, it is known that a conservative approach is safe and will be associated with lower rate of events if revascularization is finally decided.3,4 However, we do not know if FFR can also be useful for guiding the therapeutical strategy in acute coronary syndromes. The two cases presented below summarize how our FFR guided approach did not obtain adequate results.
CLINICAL CASES
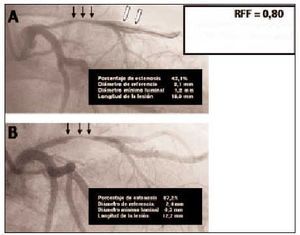
Case 1 (Figure 1)
Fig. 1. Case 1 images. A: initial angiography. Intermediate lesion of proximal anterior descending artery can be seen on left (black arrows). The white arrows indicate the pressure-guidewire distal portion. FFR determination is shown on the right. B: two months later, progression of the lesion is clearly observed (black arrows).
Male patient, 50 years old, with a single risk factor of tabaquism and without a history of previous ischemic heart disease. He was admitted due to typical chest pain at rest and subendocardial lesion electrical changes in leads II, III and aVF. Therapy with tirofiban (anti-IIb-IIIa), enoxaparin, aspirine, clopidogrel and intravenous nitroglycerin was initiated. The patient remained asymptomatic, an increase in cardiac enzymes was not detected, electrocardiographic changes reverted to normal, and after 48 h he was referred for a coronary assessment. Angiography revealed a left anterior descending artery intermediate lesion. A functional evaluation of the lesion with a pressure-guidewire (WaveWire, Endosonics, Rancho Cordova, USA) was decided. Its usage has already been described exhaustively.5 The hyperemic stimulus was generated by means of a 30-60 µg adenosine intracoronary injection. FFR determined was 0.80 repeatedly. A conservative approach was decided after this functional result, and maintaining long-term double antiaggregation with aspirine and clopidogrel was recommended.
The patient remained asymptomatic during 2 months approximately, and was after readmitted due to another unstable angina episode. Angiography revealed an evident progression of the left anterior descending artery lesion already detected. Surgical revascularization was indicated.
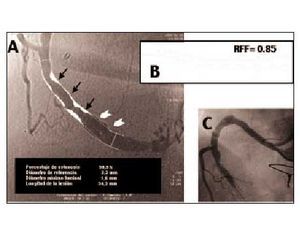
Case 2 (Figure 2)
Fig. 2. Case 2 images. A: initial situation of right coronary artery; a diffuse intermediate degree intra-stent restenosis is observed (black arrows). Distal to the stent, an aneurysmic area with an inner opacification linear defect suggestive of chronic dissection can be seen (white arrows). B: FFR analysis with the pressure sensor positioned distally to the aneurysmic area. C: right coronary artery acute occlusion, five days later.
Female patient, 66 years old, dislypemic, revascularized 5 years earlier, with a left internal mammary artery graft implanted to her left anterior descending artery. Three years later, she presented an inferior acute myocardial infarction and underwent primary angioplasty with stent implantation to her right coronary artery. Later on, while she was on nitrates, beta blockers, statin and aspirin therapy, the patient complained of repeated chest pain episodes. A stress echocardiography was performed, which was negative to any stress-induced alterations in regional wall-motion. A new angiographic study was indicated due to clinical persistence of symptoms, and an intermediate degree intra-stent restenosis of the right coronary artery was demonstrated, as well as an aneurysmatic distal portion of the artery showing a chronic dissection image. A WaveWire® pressure-guidewire study was performed, using 140 µg/kg/min doses of intravenous adenosine for this case. The pressure sensor was positioned distally to the dissected area, and after 2 min of adenosine perfusion, the pressure-guidewire was removed automatically at 0.5 mm/s while FFR was registered continuously. FFR value was 0.85 at the most distal portion. It was decided to continue conservative treatment.
After 5 days, the patient was admitted due to inferior region reinfarction and underwent another primary angioplasty of the right coronary artery, occluded at the stent area. The artery was re-opened successfully by implanting three sequential stents.
DISCUSSION
In both cases, a conservative strategy based on FFR results was inadequate. The value of FFR as a diagnostic and prognostic tool for guiding intervention of intermediate lesions is confirmed in several studies. It has been confirmed that dilating lesions with a FFR>=0,753,4 in a clinically stable population is inconvenient. The real scenario of the pressure-guidewire is somewhat different, as it is used nearly exclusively for unstable angina,6 a situation for which FFR prognostic value has not been established. Unstable angina lesions are characterized by dynamism, with the variable pressure gradient as a function of the thrombotic component and vasomotor reactivity.7 Also, the microvascular dysfunction present in acute coronary syndromes can limit adenosine vasomotor capacity, leading to an overestimation of the FFR value.
Both patients presented an acute coronary syndrome. In the first case, the initial angiographic and functional study was performed in the situation of a stabilized lesion that was possibly already more severe. In the second case, although the procedural influence in outcome of a lesion cannot be discarded, complexity due to the presence of an aneurysmic area and distal dissection could justify progression to acute occlusion, despite the absence of a significant translesional gradient. The FFR measurements in both cases disclosed an absence of a significant stenosis when performing the study. But the conservative approach resulted in an impaired outcome.
Before other studies for defining the acute coronary syndrome FFR appear, our conclusion about both cases is to be suspicatious about FFR prognostic assessment in this context. Before deciding the therapeutical approach, other occlusive severity factors (clinical, electrocardiographic, enzymatic) not related with translesional gradient should also be considered.
Correspondence: Dr. R.J. Ruiz-Salmerón.
Departamento de Cardiología Intervencionista. Hospital do Meixoeiro.
Apartado Oficial, s/n. 36200 Vigo. España.
E-mail: rafael.ruiz.salmeron@sergas.es
Received 11 July 2002.
Accepted for publication 4 October 2002.