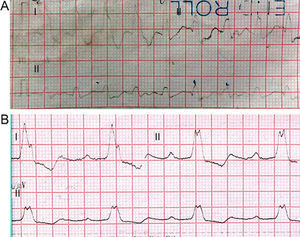
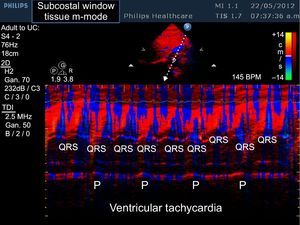
A 60-year-old, hypertensive female with chronic coronary disease was seen at the Emergency Department after she had been suffering from palpitations for three hours with a heart rate of 159 bpm; she was haemodynamically stable and the rest of the physical examination did not provide further information. Electrocardiogram: heart rate 150 bpm, QRS axis –10°, P waves not visible, QRS 0.20 ms and complete left bundle branch block (Figure 1A). After cardioversion, the electrocardiogram showed first degree atrioventricular block plus complete right bundle branch block and a heart rate of 50 bpm. Subsequent electrocardiograms showed first degree atrioventricular block plus complete left bundle branch block (Figure 1B). Ventricular tachycardia was suspected due to the patient's history of ischaemic heart disease, but the electrocardiogram diagnosis was unclear. The diagnosis of the electrophysiologist was atrial tachycardia with aberrant conduction based on the absence of haemodynamic decompensation and the similarity of the complete left bundle branch block complexes with the wide QRS tachycardia complexes. We decided to implant a pacemaker and to increase the doses of the antiarrhythmic drugs amiodarone and beta-blockers. During the echocardiography, the patient presented with tachycardia without haemodynamic instability, and views of the atria and ventricles (Figures 2A and 2B) were therefore taken in tissue M-mode via the subcostal window as well as an image that cut through the left atrium and right ventricle (Figure 3), establishing a diagnosis of VT, which was subsequently confirmed by remote pacemaker monitoring. The frequency of the episodes of ventricular tachycardia diminished with sotalol.
ISSN: 1885-5857
Impact factor 2024
4.9