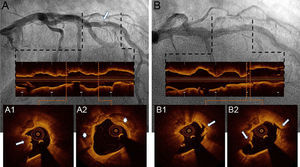
A 61-year-old man presenting with effort angina refractory to treatment underwent coronary angiography demonstrating a severely calcified obstructive lesion in the mid-segment of the left anterior descending artery (Figure 1A). Optical coherence tomography (OCT) detected severe circumferential calcification (Figure 1A, asterisks), with a calcium nodule protruding into the lumen (Figure 1A, arrow, and ) and a minimal luminal area of 2.4mm2.
Due to the severe calcification, excimer laser coronary atherectomy (ELCA) was undertaken. With a 1.4mm ELCA catheter (Spectranetics, Colorado Springs, Colorado, United States) using an energy of 60mJ/mm2 at a pulse repetition rate of 40Hz, we delivered approximately 4000 pulses over 10 runs. The OCT post-ELCA showed calcium fracture and multiple dissection planes, extending deeply into calcified plaque, with irregular intraluminal interface and an increase in minimal luminal area (3.4mm2) (Figure 1B arrows and ).
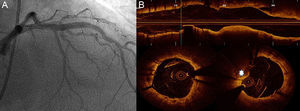
Following predilatation with a 3.5-mm noncompliant balloon, a drug eluting stent (3.5 x 20mm Xience, Abbot Vascular) was implanted, with good angiographic result (Figure 2A). Optical coherence tomography showed good expansion and apposition, with a minimal prolapse of calcified plaque towards vessel lumen (Figure 2B, asterisks).
This case shows the effect of ELCA on coronary calcified plaques assessed by OCT, and its utility in modifying the plaque and facilitating stent expansion.
CONFLICTS OF INTERESTA. Sánchez-Recalde is Associate Editor of Revista Española de Cardiología.