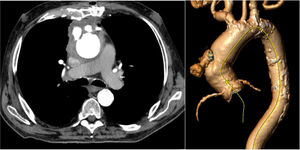
An 80-year-old man, with multiple comorbidities and history of aortic valve replacement and pericardial patch repair of the ascending aorta several years prior, presented to the emergency department with mild bleeding from a sternal wound and a pulsatile mass below the wound. Computed tomography showed sternal osteomyelitis, periaortic hematoma, and cutaneous fistulae (figure 1). Blood tests showed raised inflammatory markers and positron emission tomography was positive for infection in the ascending aorta.
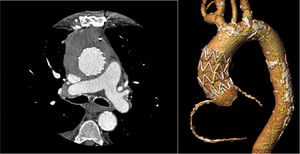
The patient was admitted to the cardiology ward, and broad-spectrum antibiotic treatment was started (piperacillin/tazobactam). A multidisciplinary meeting was held between cardiology, cardiac surgery, vascular surgery, infectious diseases, and anesthesiology. Treatment options were discussed and it was concluded that, given the patient's functional status, traditional surgery via sternotomy would have a prohibitive risk of death. It was decided to treat with endovascular exclusion of the pseudoaneurysm, planned with a 90-mm conical Relay NBS endograft (Terumo Aortic, UK). Enterococcus faecalis was isolated from blood culture and wound culture and treated with linezolid for 3 weeks prior to the intervention.
The surgery was performed without complications and the patient was discharged on oral linezolid. A year and a half later, computed tomography showed the endograft was correctly positioned and pseudoaneurysm was excluded (figure 2). Blood inflammatory markers were minimally elevated. The sternal wound remained closed, with no signs of skin inflammation.
Although endovascular surgery in such patients is not curative, it can increase life expectancy with minimal intervention. For patients with no other therapeutic option, it is worth bearing in mind as a potential treatment.
With special thanks to Patrick Bohan for his help in preparing the case.