To the Editor,
Patients with type 2 diabetes mellitus type 2 (T2DM) have a high prevalence of poor response to clopidogrel, which may contribute to their increased risk of recurrent atherothrombotic events.1 These findings underscore the need to optimize platelet inhibition in these patients.2 The OPTIMUS (Optimizing Antiplatelet Therapy in Diabetes Mellitus)-1 and -2 studies observed that a high clopidogrel maintenance dose regimen (150mg/day)3 and adjunctive cilostazol therapy (100mg twice daily),4 respectively, were associated with greater platelet P2Y12 inhibition compared with standard clopidogrel therapy (75mg/day) in T2DM patients. However, it is unknown which of these is more effective in inhibiting P2Y12 signaling in T2DM patients with suboptimal response to standard dosing. The aim of this investigation was to compare the magnitude of P2Y12 inhibitory effects of high maintenance dose clopidogrel and adjunctive cilostazol therapy among T2DM patients with stable coronary artery disease presenting with suboptimal clopidogrel response.
This analysis includes subjects with suboptimal clopidogrel response, while on dual therapy with acetylsalicylic acid and clopidogrel 75mg daily for at least 30 days, randomized in the OPTIMUS-1 and -2 trials. Details of the inclusion/exclusion criteria for the trials have previously been published.3, 4 For the purpose of this analysis, patients from both studies with suboptimal response defined according to their P2Y12 reactivity index (PRI), the most specific marker of P2Y12 mediated signalling, were analyzed. PRI values were obtained with flow cytometric analysis of the status of phosphorylation of the vasodilator-stimulated phosphoprotein according to standard protocols.3, 4 A cut-off value of PRI >50% was considered to define suboptimal responders, which reflects a consensus definition as this has been associated with an increased risk of atherothrombotic events.1, 2.
Statistical comparison of PRI continuous values was conducted using a general linear model with treatment as a fixed effect, subject as a random effect, and baseline PRI value as a covariate. Results are reported as least squares mean±standard error of the mean. Chi-square test or Fisher's exact test (according to application conditions) was used to compare the percentage of clopidogrel responders between treatments (dichotomic variable).
A total of 30 patients with suboptimal clopidogrel response treated with either adjunctive cilostazol therapy (n=15) or high maintenance dose clopidogrel (n=15) were identified. There were no differences in baseline characteristics between groups (data not shown). PRI values prior to treatment assignment were also similar (67.5±2.1 vs 70.6±2.8; P=.404).
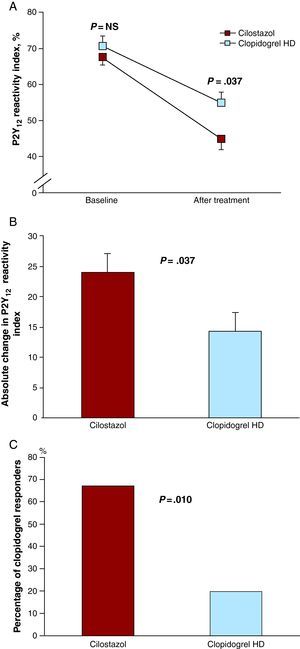
Both treatments were effective in reducing PRI (P<.001 for both). However, patients treated with cilostazol had lower PRI compared with 150mg clopidogrel (45.1±3.1 vs 54.8±3.1; P=.037; Figure 1A). The absolute change in PRI was 24.0±3.1 for cilostazol and 14.2±3.1 for the high maintenance dose clopidogrel (P=.037), leading to an absolute 9.7% (confidence interval 95%: 0.7%-18.9%) greater decrease in PRI with cilostazol (Figure 1B). Accordingly, the prevalence of suboptimal responders was also significantly lower using cilostazol (20% vs 66.7%; P=.010; Figure 1C).
Figure 1. A, Platelet reactivity at baseline and after intervention. B, Absolute change in P2Y12 reactivity index. C, Percentage of clopidogrel responders after treatment. P2Y12 reactivity index values are expressed as least square means. Error bars indicate standard errors of the mean. Garnet boxes: Cilostazol 100mg twice daily for 14 days in addition to standard dual antiplatelet therapy with acetylsalicylic acid (81mg daily) and clopidogrel (75mg daily). Blue boxes: High maintenance clopidogrel dose (150mg daily) for 30 days in addition to acetylsalicylic acid (81mg daily).
The present investigation shows that among T2DM patients with poor response to standard dual antiplatelet therapy (DAPT), the adjunctive use of cilostazol (also known as “triple therapy”) is associated with a greater magnitude of P2Y12 inhibitory effects compared with high maintenance dose clopidogrel. Importantly, levels of platelet reactivity and the prevalence of suboptimal responders are markedly lower with triple therapy. This may explain why adjunctive cilostazol therapy is more effective than DAPT in reducing atherothrombotic events, particularly in patients with DM.2 On the contrary, high maintenance dose clopidogrel is still associated with a high prevalence of poor responders, which may also explain why this strategy has failed to ameliorate outcomes.2 Our results are in line with those obtained in an unselected cohort of patients.5.
Indeed, strategies using novel P2Y12 receptor antagonists, such as prasugrel, enhance platelet inhibition in patients with DM.6 These may also explain the pronounced benefit of prasugrel in DM patients.2 However, prasugrel is associated with increased bleeding, which does not occur with adjunctive cilostazol therapy.1, 2 Notably, many DM patients also have a history of a prior cerebrovascular event, a contraindication for prasugrel use, whereas cilostazol has shown to be safe and efficacious.
We acknowledge the inherent limitations of this investigation as being a post-hoc retrospective analysis. Indeed, a prospective randomized study is warranted to confirm our findings. In addition, the clinical implications of such treatment remain elusive, underscoring the need for further investigations to test its safety and efficacy.
.
Corresponding author: dominick.angiolillo@jax.ufl.edu