The Life's Simple 7 strategy of the American Heart Association proposes 7 metrics of ideal cardiovascular health: body mass index (BMI) <25mg/m2, not smoking, healthy diet, moderate physical activity ≥ 150min/wk, total blood cholesterol <200mg/dL, systolic and diastolic blood pressures <120 and <80mmHg, respectively, and fasting blood glucose <100mg/dL. It is important to assess the combined effect of these 7 metrics in the Spanish population. We prospectively analyzed the impact of baseline Life's Simple 7 metrics on the incidence of major cardiovascular events in the PREDIMED cohort (57.5% women, average baseline age, 67 years).
MethodsThe healthy diet metric was defined as attaining ≥ 9 points on a validated 14-item Mediterranean diet adherence screener. An incident major cardiovascular event was defined as a composite of myocardial infarction, stroke, or cardiovascular death. Cox regression was used to calculate multivariable adjusted hazard ratios (HR) and their 95% confidence intervals (95%CI) for successive categories of health metrics.
ResultsAfter a median follow-up of 4.8 years in 7447 participants, there were 288 major cardiovascular events. After adjustment for age, sex, center, and intervention group, HRs (95%CI) were 0.73 (0.54-0.99), 0.57 (0.41-0.78), and 0.34 (0.21-0.53) for participants with 2, 3, and ≥ 4 metrics, respectively, compared with participants with only 0 to 1 metrics.
ConclusionsIn an elderly Spanish population at high cardiovascular risk, better adherence to Life's Simple 7 metrics was progressively associated with a substantially lower rate of major cardiovascular events.
Keywords
Cardiovascular diseases (CVDs) are the leading cause of mortality in Spain, accounting for 29% of all deaths in 2015. Prevention and treatment efforts led to a 54% decrease in cardiovascular mortality from 2000 to 2015.1 There is a high prevalence of traditional cardiovascular risk factors in Spain, and the percentage of persons with controlled risk factors is far from desirable.2
Stampfer et al.3 defined 5 factors constituting a cardioprotective lifestyle: a healthy diet, consumption of the equivalent of 1 glass of wine per day, vigorous exercise for 30min per day, body mass index (BMI) <25, and not smoking. The combined presence of these factors was associated with a reduction in the incidence of ischemic heart disease in a nurses’ cohort.3 These benefits were later confirmed in men4 and in elderly persons.5 Furthermore, these factors were inversely associated with the incidence of stroke6 and diabetes.7,8
In 2010, the American Heart Association (AHA) set the goal of reducing CVD mortality by 20% in 2020 by fostering improvements in cardiovascular health and providing a positive health message. Reference to risk factors was discontinued and substituted by the concept of optimal or ideal cardiovascular health metrics. Criteria were developed based on 7 metrics, known as Life's Simple 7 (LS7), which includes 4 healthy lifestyle behaviors (maintaining a low BMI, avoiding tobacco use, following a healthy diet, and practicing physical activity) and 3 health factors (cholesterol level, blood pressure, and fasting blood glucose concentration).9 In the NHANES10 study, achieving 6 or more metrics (with respect to attaining 1 or less) was associated with a reduction in total mortality and deaths associated with CVD and ischemic heart disease. Similar decreases were seen in the EPIC-Norfolk cohort.11 These findings indicate a synergistic effect among these metrics.
In the Spanish population there have been no evaluations of this 7-metric combination in prospective cohorts, initially measured by the occurrence of major cardiovascular events. It would also be of interest to consider the Mediterranean diet (MedD) as one of these metrics (that of a healthy diet), as the PREDIMED (PREvención con DIeta MEDiterránea) trial12 found that a MedD supplemented with extra virgin olive oil or nuts led to a short-term decrease in blood pressure, triglycerides, and blood glucose values, as well as other risk factors.13–15 Furthermore, it resulted in a 30% relative reduction in the composite variable, myocardial infarction, stroke, and cardiovascular death.16
The aim of this study was to prospectively analyze the impact of the 7 metrics on the incidence of major cardiovascular events after a median follow-up of 4.8 years in the PREDIMED study population, taken as a cohort.
METHODSThe present prospective cohort study was nested within the PREDIMED trial, a randomized, controlled, parallel group, multicenter trial to evaluate the efficacy of intensive behavioral and dietary educational interventions with 2 MedDs (enriched with extra virgin olive oil or with nuts) compared with the results in a control group (assigned a low-fat diet). The primary endpoint was the incidence of major cardiovascular events (myocardial infarction, stroke, or death from cardiovascular causes). In total, 7447 participants were included: men aged 55 to 80 years and women 60 to 80 years, with no previous CVD, but at high cardiovascular risk. All participants had to have either type 2 diabetes mellitus or ≥ 3 of 6 cardiovascular risk factors (hypertension, elevated concentrations of low-density lipoprotein cholesterol together with low concentrations of high-density lipoprotein cholesterol, obesity or overweight, active smoker, and a family history of premature CVD) with previously described criteria and cutoff points.12 All individuals signed an informed consent form for participation.
In the baseline interview, pertinent analyses and measurements were carried out to assess cardiovascular risk factors and the diagnosis of hypertension, diabetes, and hypercholesterolemia, as described.12 The physical examination included weight and height, and blood pressure measurement in triplicate using an electronic device (OMRON HEM-705CP, Hofddorp, The Netherlands). Laboratory analyses were performed to determine the lipid profile and fasting glucose concentration, among other parameters. Enrollment and the intervention were performed in the health centers where participants usually consulted.
The metrics used were those described for LS79 obtained at baseline, with the healthy diet metric adapted to the MedD pattern, which was considered fulfilled when 9 or more points were obtained on the validated 14-point scale of adherence to the MedD.17 The goal for physical activity was considered to be the equivalent of 500 METs-h/wk, assessed using the validated Spanish version of the Minnesota Leisure Time Physical Activity Questionnaire.18,19
A similar adaptation was done with the metrics from the Fuster-BEWAT Score (FBS),20 which includes blood pressure, physical activity, weight, diet, and tobacco use.
The primary endpoint was a composite of major cardiovascular events: myocardial infarction, stroke, or death due to a cardiovascular cause. In the first step, 4 different information sources were used to collect these events: a) repeated contacts with the participants, b) contact with the general practitioners providing clinical care to the participants; c) yearly review of the participants; medical records, and d) contact with the Spanish National Statistics Institute to access the National Death Registry to obtain the vital status, and in deceased participants, the cause of death. Based on this documentation, which was blinded to the intervention, the metrics, and the patient's identity, an independent event adjudication committee assigned the cardiovascular events and deaths. Only those events that were definitively assigned and had occurred between 1 October 2003 and 1 December 2010 were included.
Statistical analysisEach metric was analyzed as a dichotomous variable. Depending on whether or not it conformed to the LS7 criteria, 1 point was assigned when participants fulfilled the metric and 0 when they did not. Scores were added up, and each participant could have a total of 0 to 7 points.
For the main analysis, participants were divided into 4 categories (0-1, 2, 3, and ≥ 4 metrics) according to the number of metrics they had accumulated. The upper and lower ends of the range were collapsed, as there were few participants with 0 or more than 5 metrics.
In the case of the FBS, participants were classified into 3 categories: 0-1, 2, and ≥ 3 metrics. As there were very few participants with extreme values, both the lower (0-1) and upper (3-5) ends of the range of scores were collapsed.
A descriptive statistic was performed according to the number of metrics reached for the various confounding variables, using the mean and standard deviation for quantitative variables and percentage for qualitative variables. The incidence of the primary endpoint was calculated for each of the categories.
Cox multivariate regression analysis was used to calculate the hazard ratio (HR) and 95% confidence interval (95%CI) for major cardiovascular events, adjusted by center, age, sex, and intervention group. The group with 0-1 metrics was used as the reference category. The enrollment date was considered the time of entry. The exit date was established as the time the first major cardiovascular event occurred, the time of death by another cause, the last follow-up visit, or the last annotation in the clinical records.
The predicted probability was calculated using logistic regression analysis, with a major cardiovascular event as the dependent variable and the number of metrics as the independent variable. Subsequently, a graph was designed with the predicted marginal probabilities.
The Nelson-Aalen estimator was used to compare the cumulative hazard rate function of major events occurring over time between the 4 categories of the initial analysis.
All P-values were two-tailed and significance was set at p <.05. Analyses were performed using Stata, version 12.0 (Stata Corp.; College Station, Texas, United States).
RESULTSThe 7447 participants in the PREDIMED study had a mean follow-up of 4.8 years; that is, 31 980 person-years. During this period, there were 288 major cardiovascular events.
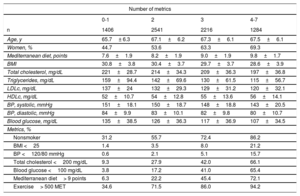
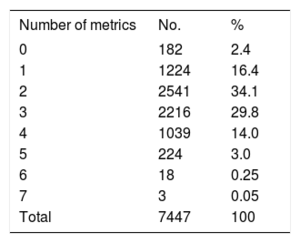
The general data according to the number of LS7 metrics are shown in Table 1. In all cases, the values for glucose, lipids, systolic and diastolic arterial pressure, the BMI, MedD adherence, and percentage of women gradually increased as the number of metrics increased. Among the total number of participants, 73% performed the recommended exercise, 61.3% were nonsmokers, 35% had a blood cholesterol value <200mg/dL, 34.5% fulfilled more than 9 points on the MedD pattern, 30% had a glucose concentration <100mg/dL, 7.5% had a BMI <25%, and 5% had blood pressure <120/80mmHg.
Distribution of the general characteristics of the sample by number of metrics
| Number of metrics | ||||
|---|---|---|---|---|
| 0-1 | 2 | 3 | 4-7 | |
| n | 1406 | 2541 | 2216 | 1284 |
| Age, y | 65.7± 6.3 | 67.1±6.2 | 67.3±6.1 | 67.5±6.1 |
| Women, % | 44.7 | 53.6 | 63.3 | 69.3 |
| Mediterranean diet, points | 7.6±1.9 | 8.2±1.9 | 9.0±1.9 | 9.8±1.7 |
| BMI | 30.8±3.8 | 30.4±3.7 | 29.7±3.7 | 28.6±3.9 |
| Total cholesterol, mg/dL | 221±28.7 | 214±34.3 | 209±36.3 | 197±36.8 |
| Triglycerides, mg/dL | 159±94.4 | 142±69.6 | 130±61.5 | 115±56.7 |
| LDLc, mg/dL | 137±24 | 132±29.3 | 129±31.2 | 120±32.1 |
| HDLc, mg/dL | 52±10.7 | 54±12.8 | 55±13.6 | 56±14.1 |
| BP, systolic, mmHg | 151±18.1 | 150±18.7 | 148±18.8 | 143±20.5 |
| BP, diastolic, mmHg | 84±9.9 | 83±10.1 | 82±9.8 | 80±10.7 |
| Blood glucose, mg/dL | 135±38.5 | 126±36.3 | 117±36.9 | 107±34.5 |
| Metrics, % | ||||
| Nonsmoker | 31.2 | 55.7 | 72.4 | 86.2 |
| BMI <25 | 1.4 | 3.5 | 8.0 | 21.2 |
| BP <120/80 mmHg | 0.6 | 2.1 | 5.1 | 15.7 |
| Total cholesterol <200 mg/dL | 9.3 | 27.9 | 42.0 | 66.1 |
| Blood glucose <100 mg/dL | 3.8 | 17.2 | 41.0 | 65.4 |
| Mediterranean diet> 9 points | 6.3 | 22.2 | 45.4 | 72.1 |
| Exercise> 500 MET | 34.6 | 71.5 | 86.0 | 94.2 |
BMI, body mass index; BP, blood pressure; HDLc, high density lipoprotein cholesterol; LDLc, low density lipoprotein cholesterol.
Unless otherwise indicated, values are expressed as the mean ±standard deviation.
Among the total, 0.04%, 0.2%, and 3% of participants achieved 7, 6, and 5 metrics, respectively (Table 2).
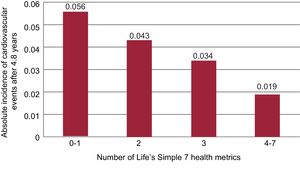
The absolute incidence of events at 5 years was lowest in the category with the largest number of metrics, and the incidence decreased as the number of metrics increased (Figure 1).
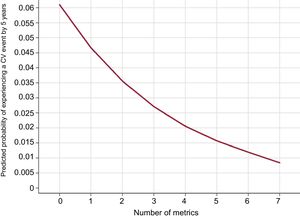
The predicted probability of experiencing a cardiovascular event by 5 years of follow-up was inversely related to the number of metrics attained (Figure 2).
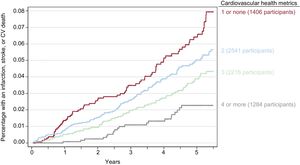
The curves showing the estimated percentage of participants with some type of major cardiovascular event in the 4 categories of metrics showed a significant separation during follow-up that was evident starting from the first year (Figure 3).
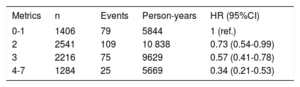
After adjustment for age, sex, center, and intervention group, participants with 2, 3, and 4 or more LS7 metrics had a significantly lower risk of developing a major cardiovascular event—HR=0.73 (95%CI, 0.54-0.99), HR=0.57 (95%CI, 0.41-0.78) and HR=0.34 (95%CI, 0.21-0.53), respectively—than those with 0 or 1 metrics (Table 3).
Risk of cardiovascular events according to the number of health metrics divided into 4 categories and adjusted by center, sex, age, and intervention group
| Metrics | n | Events | Person-years | HR (95%CI) |
|---|---|---|---|---|
| 0-1 | 1406 | 79 | 5844 | 1 (ref.) |
| 2 | 2541 | 109 | 10 838 | 0.73 (0.54-0.99) |
| 3 | 2216 | 75 | 9629 | 0.57 (0.41-0.78) |
| 4-7 | 1284 | 25 | 5669 | 0.34 (0.21-0.53) |
95%CI, 95% confidence interval; HR, hazard ratio.
As to the FBS, participants with 2 and ≥ 3 metrics had a significantly lower risk of experiencing a major cardiovascular event, with HR=0.71 (95%CI, 0.55-0.92) and HR=0.49 (95%CI, 0.33-0.73), respectively, than those with 0 or 1 metrics.
DISCUSSIONA strong inverse association was found between the number of ideal cardiovascular health metrics, assessed according to the LS7 strategy, and the incidence of CVD. The impact of these healthy lifestyle habits together with favorable lipid, blood pressure, and glucose values in reducing the incidence of major cardiovascular events was striking, even in this cohort at high cardiovascular risk. The LS7 is suitable for use in the Spanish population with this profile, and it is of considerable interest for the prevention of cardiovascular events in primary care and other clinical settings attending these patients. The present findings underscore the need to focus efforts on these 7 points, but further investigation is required to determine whether these results can be reproduced in populations at moderate and low cardiovascular risk.
LS7 metrics were only measured at baseline, before the intervention in the PREDIMED study; hence, the absolute incidence rates of events may have been influenced by the nutritional intervention and were likely optimistic. However, as both the intervention group and controls were recommended diets considered to be heart-healthy, this situation would have occurred in both groups. Irrespective of this consideration, as the results were adjusted by the intervention, the HRs would continue to be valid.
One differential element in this study regarding the LS7 and FBS criteria is that a healthy diet was considered to be one scoring more than 9 points on the 14-point questionnaire of adherence to the MedD pattern,18 validated by the PREDIMED group. We believe that application of this level of adherence, proven to be protective against CVD, as the marker of a heart-healthy diet is an important contribution of the study and one of its strong points. It provides evidence supporting systematic assessment of the MedD in all clinical settings within the basic evaluation and interventions to prevent CVD. Of note, scores for this metric would likely be high in the Spanish population and more difficult to achieve in non-Mediterranean populations with other dietary habits.21
The percentage of participants reaching 7, 6, and 5 metrics in the present study was very low and consistent with the selection criteria, as all individuals were at high cardiovascular risk. This circumstance can lead to underestimation of the prevalence of healthy lifestyle habits in comparison to that of the general population. Thus, the present results are lower than those obtained in Spain by Graciani al.,22 in a general population sample of 11 408 persons with no previous CVD older than 18 years, participating in the ENRICA study. The percentage of individuals with 7, 6, or 5 LS7 metrics in that study was 0.2%, 3.4% and 5.3%, respectively. However, it is noteworthy that only 11.1% of individuals adhered to the ideal diet based on criteria defined by the AHA vs 34% of the present sample with more than 9 points of the MedD pattern. This difference may have arisen because of greater adherence to the MedD in a sample of older persons such as the PREDIMED population, which, in addition to having a more heart-healthy diet, had received more intense counselling on the proper diet for controlling their cardiovascular risk factors. Other international studies, such those by Folsom et al.23 performed in the United States and Bi et al.24 in China, also reported low percentages of persons with an ideal level of cardiovascular health: 0.1% and 0.2%, respectively. Nonetheless, these percentages are still higher than the 0.04% found in our study. The participants included were a population aged 40 to 65 years in the study in the United States and a general population older than 20 years in the Chinese study. Despite the peculiarities of the present study population—advanced age and at high cardiovascular risk—the extremely low percentage of participants with optimal cardiovascular health is alarming.
The results found are in line with those of previous studies in other countries that have demonstrated the morbidity and mortality-related benefits of gaining a large number of components of cardiovascular health.11,12 A recent meta-analysis confirmed the association between a greater number of LS7 metrics and a reduction in the incidence of CVD and all-cause mortality.25 Furthermore, the presence of these favorable lifestyle habits in middle age is associated with less severe disability in advanced ages.26
In an interventional study applying an overall approach to cardiovascular risk factors, Gómez-Pardo et al.20 proposed the use of the FBS, which collects a smaller number of metrics (blood pressure, physical exercise, weight, diet, and tobacco consumption) and excludes cholesterol and glucose determinations. This could be equally predictive of good cardiovascular health and would be much easier to perform. In the PESA cohort, Fernández-Alvira et al.,27 compared the predictive value of the FBS for cardiovascular health (but not for clinical events) with that of 7 metrics that indicate subclinical atherosclerosis in the coronary and iliofemoral arteries and the aorta. The authors concluded that the 2 scales had similar yield. The present study also analyzed these 5 FBS components, grouped into 3 categories: 0-1, 2 and > 3 metrics. Participants with 2 and> 3 FBS metrics had a lower risk of experiencing a major cardiovascular event—HR=0.71 (95%CI, 0.55-0.92) and HR=0.49 (95%CI, 0.33-0.73), respectively—than those with 0 or 1 metrics. These results are similar to those obtained for the LS7, as the confidence intervals overlap, although the point estimate of the HR was more protective for 4 or more LS7 metrics (0.34) than for 3 or more FBS metrics (0.49).
The results of the present study suggest that in addition to individual interventions of an evaluative and educational nature carried out in clinical practice, structural efforts are also essential, achieved through policies promoting cardiovascular health in the entire population. A larger number of cardiovascular events occur in persons of low or moderate cardiovascular risk simply because the prevalence of these risk categories in the population is much higher.28 Achieving advances in measuring the metrics of the general population, although they may seem modest, can have a huge impact on population health.28–30 A positive and possibly synergistic view of the benefits associated with a greater accumulation of favorable metrics can contribute to a considerable improvement in cardiovascular health and have positive repercussions on preventing other health problems, and on disability, longevity, and quality of life, as well as on the economic development of individuals, families, and society as a whole.
These efforts should take into account “the determinants of the classic determinants” of CVD; that is, the behaviors that are the basis for their development and can be modified by simple aspects of lifestyle. These determinants, which do not require inclusion of traditional risk factors or medication use, include maintaining an appropriate body weight, having an active lifestyle, spending less time watching television, adapting to the Mediterranean pattern of alcohol consumption, devoting more time to friends, and following a suitable work schedule. In the SUN cohort of university graduates, Díaz-Gutiérrez et al.31 found that a healthy lifestyle that did not require measurement of lipids, blood pressure, or glucose and was defined by 10 points including the aforementioned factors, was associated with a lower risk of CVD. A 78% reduction in the relative risk of a first cardiovascular event was found between the highest scores (7-10 points) and the lowest scores (0-3 points) after a median follow-up of 10.4 years.
The currently ongoing PREDIMED-Plus study32–34 is attempting to go further, investigating a MedD pattern with caloric restrictions and enhanced physical exercise vs a MedD regimen without these elements. An even greater direct impact on the LS7 metrics is expected from this intervention.
Lastly, it should be noted that within its National Health System, Spain has one of the most highly developed primary care schemes in the world, which guarantees equitable access to high-quality health care for the entire population. Because of their proximity to the patients, primary care physicians, pediatricians, and nurses working in primary care are in a privileged position to have an impact on fomenting healthy behavior, simultaneously with other actions in the community. Once risk factors are detected, interventions can be applied at the individual and community level.
FUNDINGThis study was funded by the Instituto de Salud Carlos III, Spanish Ministry of Health through the support provided to research networks especially developed for the study (RTIC G03/140, to R. Estruch and RTIC RD 06/0045 to M.Á. Martínez González), the Biomedical Research Networking Center for Physiopathology of Obesity and Nutrition, the Spanish National Center for Cardiovascular Research (CNIC 06/2007), Spanish Health Research Fund-European Fund for Regional Development (PI04-2239, PI05/2584, CP06/00100, PI06/00100, PI07/0240,PI07/1138, PI07/0473, PI10/01407, PI10/02658, PI11/02505), Ministry of Science and Innovation (AGL-2009-13906-C02 and AGL-2010-22319-C03), Mapfre Foundation 2010, Regional Health Ministry of Andalusia (PI0105/2007), Public Health Division of the Department of Health of the Generalitat of Catalonia and Generalitat of Valencia (ACOMP06109, GVACOMP201-181,GVACOMP2011-151, CS2010-AP-111, and CS2011-AP-042), and the Regional Government of Navarre (P27/2011).
CONFLICTS OF INTERESTNone declared.
- –
Good cardiovascular health is directly related to 4 heart-healthy behaviors: low BMI, no smoking, healthy diet, and physical activity, and to 3 health factors within normal limits: cholesterol, blood pressure, and fasting blood glucose.
- –
The AHA included these 7 metrics (LS7) in a strategy aimed at achieving a 20% reduction in cardiovascular mortality by 2020 in the United States.
- –
In the Spanish population, despite an observed decrease in cardiovascular morbidity and mortality, the metrics of good cardiovascular health are far from desirable levels.
- –
The impact of the 7 metrics was investigated in a prospective analysis of a cohort at high cardiovascular risk from the PREDIMED study, considering the healthy diet metric to be a MedD pattern. A strong inverse association was found between the number of LS7 metrics achieved and the incidence of major cardiovascular events.
- –
Use of the LS7 metrics is appropriate for a Spanish population at high cardiovascular risk. This study supports the need to enhance efforts on these 7 points for the prevention of cardiovascular events in the primary care area and all other health settings that provide care to these high-risk patients.