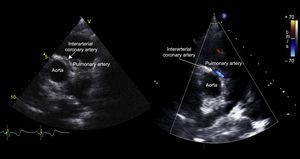
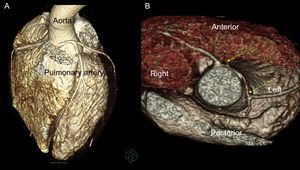
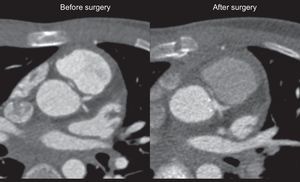
A 12-year-old boy with no relevant personal or family history experienced syncope with cardiorespiratory arrest and ventricular fibrillation while playing basketball. He was admitted to the intensive care unit for monitoring and assessment of idiopathic ventricular fibrillation. An echocardiogram was recorded and reverse interarterial flow was observed in color Doppler mode. A left coronary artery originating in the right coronary sinus was detected following an interatrial path (Figure 1). A left coronary artery was not observed in the usual sinus. Severe systolic and diastolic dysfunction of the left ventricle was observed, with elevated markers of cardiac ischemia (troponin, 6 ng/mL; creatine kinase MB isoenzyme, 158μg/L), and ST depression in leads DII, DIII, aVF, and V2-V6 in the electrocardiogram. He required inodilator support for 9 days and was then switched to oral treatment with angiotensin converting enzyme inhibitors and β blockers. Cardiac computed tomography was performed to complete the study and this technique confirmed the echocardiographic findings (Figure 2A); of note was a narrowing of the left main coronary artery, attributed to intramural aortic pathway, with widening once more at the bifurcation (indicated with the yellow arrows in Figure 2B). During surgery, fenestration of the aortic lumen was performed with the distal coronary lumen of the left main coronary artery opening the intramural coronary artery up to the commissure (yellow arrows in Figure 3). There were no complications after surgery. After 3 years of follow-up, the outcome was satisfactory; the patient remained clinically asymptomatic, with full recovery of ventricular function. Single photon emission tomography during exercise showed minimal anteroapical necrosis, with no signs of ischemia.10.1016/j.recesp.2017.05.022
ISSN: 1885-5857
Impact factor 2024
4.9