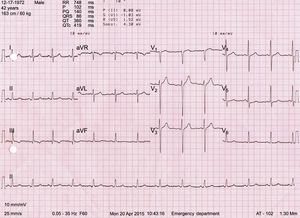
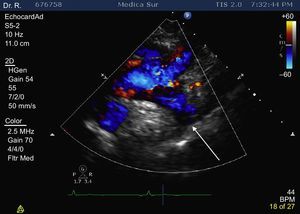
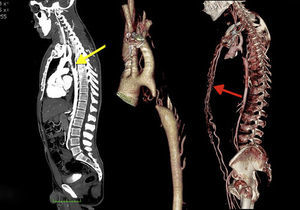
A 42-year-old man, with previous hypertension (190/100mmHg), attended the emergency department complaining of chest tightness, with pain radiating to his neck and left shoulder. The initial electrocardiogram revealed sinus rhythm, with no signs of ischemia, infarction, or left ventricular hypertrophy (Sokolow-Lyon index, 25mm; Cornell voltage criteria, 2.5mV) (Figure 1); the cardiac troponin I level was high (1.47 ng/mL). Transthoracic echocardiography showed normal mobility and left ventricular function, and there was mild left ventricular hypertrophy and bicuspid aortic valve, with no evidence of stenosis and/or regurgitation. Color Doppler (suprasternal view) revealed interruption of the blood flow at the level of the aortic arch, distal to the origin of the left subclavian artery (Figure 2, arrow). Computed tomography angiography corroborated the interruption of the aortic arch distal to the origin of the left subclavian artery (Figure 3, yellow arrow).
Interrupted aortic arch is a rare congenital heart defect (< 1%) characterized by a complete lack of luminal continuity between the ascending and descending aorta. In adults, type A is located just beyond the left subclavian artery (79%); type B, between the left carotid artery and the left subclavian artery (16%); and type C, between the innominate artery and the left carotid artery (3%). Individuals with type A may develop adequate collateral circulation, which mitigates severe symptoms and explains why they are able to live to adulthood. Type A may represent the final stage of progressive aortic coarctation with development of significant collateral circulation, as was found in this patient (Figure 3, red arrow).