A 69-year old man with no relevant medical history was admitted for acute pulmonary edema and cardiogenic shock, caused by tearing of the posterior papillary muscle secondary to acute inferior myocardial infarction. The patient underwent emergency surgery with implantation of a mitral bioprosthesis and bypass grafting of the left anterior descending artery to the left mammary artery.
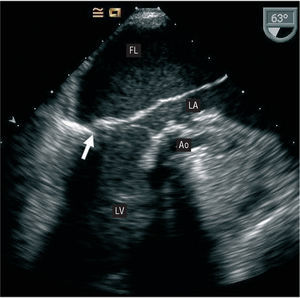
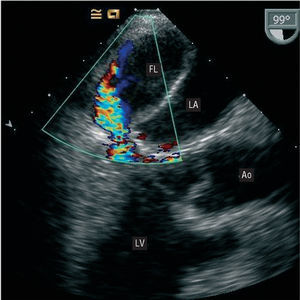
During the immediate postoperative period, the patient experienced hemodynamic instability and difficulty weaning from the intra-aortic contrapulsation balloon. On transthoracic echocardiography, the mitral prosthesis showed no alterations and left ventricular systolic function was preserved. Because there was no correlation between the transthoracic echocardiography findings and the patient's clinical status, transesophageal echocardiography was performed. The examination revealed a false chamber in the interior of the left atrium that was formed by the dissected posterior atrial wall and occupied nearly the entire true lumen (Figure 1). In addition, retrograde systolic flow was observed in the interior, coming from the posterior wall of the left ventricle below the prosthesis. There was no evidence of a communication between the true and false lumen, or perivalvular regurgitation (Figure 2).
Figure 1.
Figure 2.
The patient underwent another procedure. The prosthesis was removed and a laceration was discovered in the left ventricular wall that served as the entry portal of the false chamber comprised of the posterior wall of the dissected left atrium. The left ventricular tear was repaired with autologous pericardium and a mechanical mitral prosthesis was implanted. The postoperative course was favorable, and on day 12 following the operation the patient was discharged. Four months later his clinical status was NYHA Class I.