We present the case of a 46-year-old woman who attended the emergency department with New York Heart Association (NYHA) class II-III dyspnea, dry cough, orthopnea, and generalized edema. Physical examination revealed bibasilar crackles and pitting edema in the lower limbs. Electrocardiography demonstrated sinus rhythm at 95 bpm and incomplete right bundle branch block. Chest radiography showed congestive signs, blood tests detected elevated natriuretic peptide levels, and focused cardiac ultrasound identified right heart dilatation. Computed tomography (CT) angiography of the pulmonary arteries ruled out a pulmonary thromboembolism and the patient was admitted to the cardiology department.
During hospitalization, the patient improved in response to diuretic therapy. A comprehensive echocardiogram showed right heart dilatation and signs of pulmonary arterial hypertension (PAH) (figure 1A). Right heart catheterization revealed a mean pulmonary artery pressure of 25mmHg. The remaining parameters were normal and a vasoreactivity test was negative. Because pulmonary disease was ruled out using chest CT and spirometry, the PAH was classified as primary idiopathic PAH. The patient was discharged on sildenafil 20mg/12h and furosemide 40mg/8h.
A: initial transthoracic echocardiography (TTE); right heart dilatation, tricuspid valve without vegetation, mild tricuspid regurgitation (TR), and elevated tricuspid regurgitation velocity as an indirect sign of pulmonary arterial hypertension. B: TTE after diagnosis of Whipple disease; vegetation on the septal leaflet of the tricuspid valve (arrows) and severe TR. C: follow-up TTE; reduced vegetation size (arrows). D: 1-year TTE, after treatment completion; retracted septal leaflet (arrow) with severe residual regurgitation and normal regurgitation velocity.
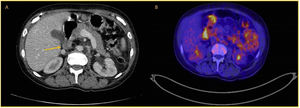
Two months later, she was admitted with asthenia, anorexia, weight loss of 15kg, and early satiety; notable findings included hemoglobin of 9mg/dL, but no gastrointestinal bleeding. No cardiac decompensations had occurred since the previous hospitalization and the patient was free from edema and dyspnea at admission. A neoplastic condition was suspected. Abdominal CT demonstrated an increase in the thickness of the third duodenal portion and multiple mesenteric and retroperitoneal adenopathies, findings suggestive of lymphoma (figure 2A). Upper gastrointestinal endoscopy, colonoscopy, and positron emission tomography (PET)-CT were performed. Endoscopy showed a thickened, edematous, and friable duodenojejunal mucosa, with multiple lymphangiectasias and petechiae and ecchymosis in the biopsied tissue. The PET-CT revealed inflammatory or infectious findings of unclear significance (figure 2B). Intestinal biopsy demonstrated infiltration of the lamina propria by foamy histiocytes, which were stained by periodic acid-Schiff (PAS) stain, a finding compatible with Whipple disease (WD). Fecal polymerase chain reaction (PCR) was positive for Tropheryma whipplei (TW). Cerebrospinal fluid (CSF) analysis ruled out a central nervous system infection. Echocardiography performed to rule out cardiac diseases secondary to WD showed mobile vegetation, attached to the septal leaflet of the tricuspid valve, and severe tricuspid regurgitation, not present in the previous analysis, compatible with tricuspid endocarditis due to WD (figure 1B). Treatment was begun with ceftriaxone i.v. 2g/24h for 4 weeks and doxycycline 100mg/12h and hydroxychloroquine 200mg/8h for 1 year; the furosemide dosage was reduced to 40mg/24h and sildenafil was maintained at 20mg/12h.
Ambulatory care was selected with echocardiographic follow-up every 3 months (figure 1C). The dyspnea resolved and the patient experienced no cardiac decompensations. Her pulmonary pressure normalized, sildenafil was withdrawn, the furosemide was maintained at 40mg/24h, and the echocardiographic evidence of PAH abated. Her pro-brain natriuretic peptide (proBNP) level was 261 pg/mL. Echocardiography at 1 year of follow-up showed a tricuspid valve with a small hyperechogenic vegetation on the septal leaflet and persistence of the severe tricuspid regurgitation (figure 1D). The patient is currently asymptomatic and remains under follow-up. The patient's legal guardian signed informed consent for publication of the case.
WD is a rare disease caused by infection with TW that has an estimated prevalence of 0.1 to 1 cases/million.1 Diagnosis is based on the presence of PAS-positive macrophages in histological samples of duodenal biopsies and on serological tests showing TW DNA in different tissues.2
WD usually presents as a triad of symptoms: fever, diarrhea, and joint pain. It can be accompanied by weight loss, chest pain, cardiac abnormalities, and manifestations affecting the central nervous system or any other organ.1
Infectious endocarditis (IE) is the most frequently associated cardiac condition,1 and TW is isolated in 5% of cases of culture-negative IE.3 The prevalence of TW-associated IE is low but its actual frequency may be higher, given that cases have been reported based on histological analysis or PCR of cardiac valves in patients not meeting the Duke criteria.4 The most frequently affected valve is the mitral valve.3 The etiological diagnosis of IE due to TW is conducted via biopsy or blood PCR.5 Its treatment is based on antibiotic therapy with doxycycline 200mg/24h and hydroxychloroquine 200-600mg/24h for at least 18 months.5
In the lungs, this condition manifests as chronic cough, dyspnea, and pleuritic pain, similar to interstitial lung disease.1 WD-associated PAH is an infrequent finding. Its pathophysiology has not been established but a proinflammatory state has been proposed, mediated by cytokines, direct infiltration of TW into the pulmonary vessels, or embolisms of PAS-positive cells.2 In our patient, PAH was initially classified as group 1,6 the changes over time in the echocardiographic parameters of the disease after antibiotic therapy led to its reclassification in group 5, as PAH with unclear and/or multifactorial mechanisms. No evidence is available on the management of pulmonary vascular disease caused by WD. However, most published cases of PAH reported resolution of PAH after antibiotic therapy, similar to what occurred in our patient. This observation supports the hypothesis of direct injury to the pulmonary vessels by the microorganism.
FUNDINGNone.
AUTHORS’ CONTRIBUTIONSI. Gallo Fernández is the main author of the article. M. Delgado Ortega supervised the manuscript and the patient diagnosis. J. Perea Armijo and J. Rodríguez Nieto collaborated on the manuscript drafting. D. Pastor Wulf and J. López Baizán collaborated on the echocardiographic follow-up studies and figure preparation.
CONFLICTS OF INTERESTNone.