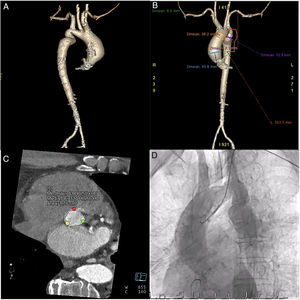
A 70-year-old man with multiple comorbidities and a diagnosis of coarctation of the aorta, severe aortic stenosis on a bicuspid valve, and a 46-mm ascending aortic aneurysm was referred for percutaneous treatment due to unacceptable surgical risk (Figure 1). His past medical history included severe peripheral vascular disease in the right lower limb with multiple surgical revascularizations, laryngeal cancer that had been treated with surgery and cervical radiotherapy with severe secondary dysphasia that required gastrectomy, and inoperable lung cancer undergoing treatment with radiotherapy.
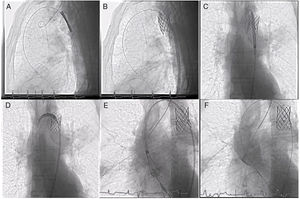
It was decided to treat both defects in a single procedure to minimize the need for vascular access and reduce the possibility of aortic dissection during the procedure due to excessive manipulation. The procedure was performed via 16 Fr left femoral access. First, we implanted a 45 mm 10 zig expanded polytetrafluoroethylene-covered stent mounted on a 22×45mm BIB (balloon in balloon) catheter, immediately distal to the left subclavian, post-dilated with a 25×50mm balloon, with a good angiographic result. We then introduced the release system for the Evolut PRO 26 self-expanding prosthetic aortic valve, crossing the stent without disrupting it, and we proceeded to implant the valve, with a good result and mild paravalvular regurgitation (Figure 2).
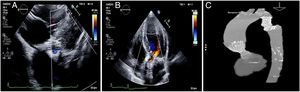
The patient progressed satisfactorily and was discharged on day 5. Radiological follow-up showed good apposition of both devices (Figure 3).
We believe that this case could be educationally informative due to its unusual nature and demonstration of a possible alternative to surgery or 2 percutaneous procedures in patients with high anesthetic or vascular risk.