A 69-year-old woman with a history of arterial hypertension, paroxysmal atrial fibrillation, giant multiperforated atrial septal aneurysm, and ischemic stroke 1 year previously, was admitted to our hospital with a new ischemic stroke episode, although she was on anticoagulant therapy with correct therapeutic index.
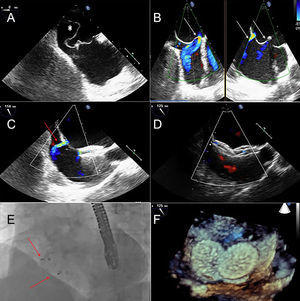
During hospital admission, the giant multiperforated atrial septal aneurysm was seen on transesophageal echocardiography (Figure A, asterisk) with a left-to-right shunt (Figure B, white arrows) at 4 levels. Although the effectiveness of percutaneous closure for preventing recurrent embolic events in this setting is not well established, we decided to perform a percutaneous closure with the atrial septal defect occluder Figulla® Flex II (Occlutech International AB, Sweden). The procedure was guided by transesophageal echocardiography (Figures C-F). Right femoral vein access was conducted in order to reach the right atrium. Afterwards, transeptal puncture with a 12F multipurpose catheter was performed and a 24-mm device was implanted. Nevertheless, we noticed that the left-to-right shunt persisted (Figure C, red arrow). To achieve total occlusion, a second 24-mm device was implanted through the septal defect without a final left-to-right shunt assessed by color Doppler (Figure D). Final apposition was confirmed by fluoroscopy (Figure E, red arrows) and 3D imaging from transesophageal echocardiography (Figure F). To avoid device-related thromboembolic events and due to the high risk of bleeding (HAS-BLED 3 points), our patient was discharged on anticoagulant therapy with dicoumarinic agents indefinitely and dual antiplatelet therapy with aspirin and clopidogrel for 1 month followed by aspirin for 5 months.