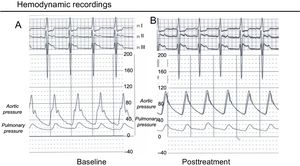
A 68-year-old man, with a bileaflet mechanical aortic valve implanted surgically in 2010, was referred for evaluation for percutaneous closure of a large paravalvular leak that was causing heart failure. Cardiac computed tomography (CT) with retrospective cardiac synchronization was performed before (Figure 1D) and after (Figure 1E-H) the procedure. The baseline CT study showed a normally-functioning prosthetic valve with a cranially-angulated (20°) annulus and a regurgitant paravalvular area of 3.42cm2 (Figure 1C in diastole and Figure 1B-D in systole; arrow, paravalvular leak). On fluoroscopy and CT, no rocking of the prosthetic valve was observed during the cardiac cycle. Hemodynamically, the aortic diastolic pressure was lower than the pulmonary systolic pressure (Figure 2A), and study confirmed severe volume overload with ventricular dysfunction (end-diastolic volume, 340mL/m2; end-systolic volume, 258mL/m2). Ejection fraction was 23%. The coronary arteries did not have significant stenosis. Two Amplatzer AVP3-145 devices (Abbott; Chicago, Illinois, United States) were implanted for percutaneous closure, with angiographic and transesophageal echocardiographic guidance.
After the procedure, aortic pressure improved, with a marked increase in diastolic pressure (Figure 2B). Postprocedure cardiac CT confirmed correct positioning of the closure devices in the angulated dehiscence (Figure 1E-G in diastole and Figure 1F-H in systole). Prior to discharge, the patient had significantly improved clinically, with no hemolysis; this lasted for 1 year after the procedure.