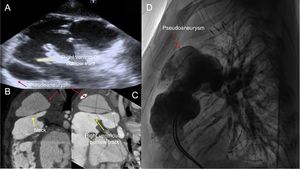
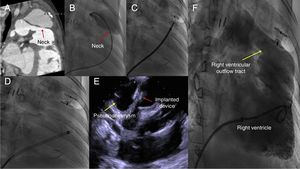
We present the case of a 46-month-old boy diagnosed with pulmonary atresia with ventricular septal defect and hypoplasia of the pulmonary branches. A neonatal systemic-pulmonary shunt was established, and at 37 months, palliative surgical repair was performed with augmentation of pulmonary branches associated with the Rastelli procedure (Contegra 12mm). Following the use of extracorporeal circulation, there were pulmonary complications with severe hypoxemia necessitating extracorporeal membrane oxygenation and stenting of the left pulmonary artery and right lobes, after which it was possible to withdraw support. During follow-up, a cavity was visualized (Figure 1) adjacent to the right ventricular outflow tract, and a giant pseudoaneurysm was observed on computed tomography (CT) and confirmed on angiography (Figure 1B, C, and D). In the absence of objective clinical data indicating active infection, we decided to use a percutaneous approach. With the help of the CT images (Figure 2), a hydrophilic guidewire was used to gain access to the cavity and advance a 6-Fr JR4 catheter (Figure 2B), which was exchanged for a specific sheath. Finally, we implanted an Amplatzer device for ventricular septal defect closure (Figure 2C and D), which achieving sealing and isolation (Figure 2E and F). However, 15 days later, the patient had fever with signs of superinfection, which was treated by surgical cleansing and substitution with a homograft and Dacron tube. Percutaneous leak closure after surgery can be an option in selected patients. However, previous screening for infectious etiology is crucial, using tests such as positron emission tomography/CT. The use of multimodal imaging is of enormous importance for successful treatment.
ISSN: 1885-5857
Impact factor 2024
4.9