Prior to the closure procedure, left atrial appendage (LAA) extreme size (< 11 or > 31mm) or thrombus should be excluded. In general terms, the landing zone is measured at the largest LAA phase from 10 to 20mm inside the left lateral ridge to 5mm inside the left circumflex artery. Currently, transesophageal echocardiography (TEE) is the most common screening technique (Figure 1A), 3-dimensional (3D) TEE measures being slightly larger (Figure 1B). Cardiac computed tomography (CT) offers superior definition and better measurement accuracy than angiography (Figure 1C). On TEE (Figure 1D), thrombus appears as a hyperechogenic space-occupying image, which can be differentiated from sludge (arrow) by employing echo-contrast. On CT (Figure 1E), thrombus appears as an arterial-phase filling defect, which is still present at venous-phase acquisition (upper), conversely to sludge (bottom).
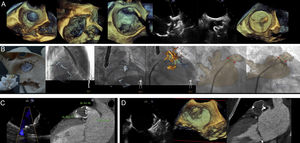
The LAA closure procedure is usually guided with TEE (Figure 2A): LAA en-face 3D-view; 3D-guided transseptal puncture; sheath inside LAA; 2-dimensional-orthogonal views (45° to monitor the circumflex artery and 135° to supervise the deployment depth); and device prior to being released. Some new imaging techniques are helpful complements (Figure 2B). Through the use of 3D-printed models, the LAA can be assessed easily, and it is also possible to assay deployment. Likewise, TEE or CT fusion imaging improves spatial comprehension.
According to imaging follow-up, residual leak (Figure 2C) can be difficult to identify with TEE. On CT, it appears as LAA contrast enhancement distal to the closure device. Thrombus (Figure 2D) can be identified on the external device surface on TEE as an irregular hyperechogenic structure, or as a low attenuation defect on CT.
Conflicts of InterestI. Cruz-González is proctor for St Jude Medical and for Boston Scientific.