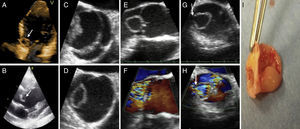
A 28-year-old man with no relevant medical history was admitted to our hospital for fever occurring early in the evening, weakness, dyspnea, and headache of 2 months’ duration. Blood culture was persistently positive for Streptococcus sanguinis (5/5). Upon admission, a diastolic murmur that had not been detected previously was found. Transthoracic echocardiography was performed and showed a large aneurysm in the noncoronary leaflet of a bicuspid aortic valve, severe aortic insufficiency, and left ventricular dilation (Figures A and B). Transesophageal echocardiography identified perforation of the aneurysm as the cause of aortic insufficiency (Figures C-H). After the patient had completed antibiotic treatment and blood cultures tested negative, a decision was made to operate due to persistent dyspnea in the presence of severe aortic insufficiency. The same findings were observed (Figure I) as described above.
Aortic valve aneurysms are rare, with fewer than 15 cases reported in the literature. Although the most probable cause is infectious endocarditis, this disease has been demonstrated in only a few cases. Our case met 2 of the major Duke criteria and 2 minor criteria for the diagnosis of definite infectious endocarditis: positive blood culture, new valvular insufficiency, fever, and predisposing heart disease. Ultimately, the valve culture was sterile, but surgery was done after completing antibiotic treatment and achieving negative blood cultures.
As in other published cases, there was an absence of characteristic images of endocarditis accompanying the aneurysm. Therefore, an isolated finding of aortic aneurysm advises assessing for infectious endocarditis to rule out the presence of this condition.