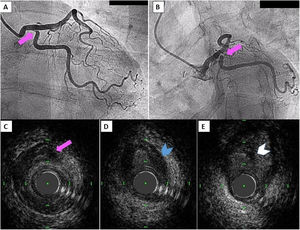
A 50-year-old woman with no known cardiovascular risk factors was admitted to the emergency department due to acute chest pain. No ST-segment deviations were found on electrocardiography. Transthoracic echocardiography revealed preserved left ventricular ejection fraction and inferolateral hypokinesia. Troponin I was increased to 2670 ng/L. Coronary angiography showed no atherosclerotic-pattern but revealed a «ring sign» at the ostium of the circumflex, which was verified in 2 different projections (figure 1A,B, arrows, videos 1 and 2 of the supplementary data). Based on the clinical profile, spontaneous coronary artery dissection (SCAD) was suspected, although the angiogram showed no classic, specific sign. Therefore, intravascular ultrasound (IVUS) (video 3 of the supplementary data) was performed to better identify the etiology, revealing a normal 3-layer vessel with no atherosclerotic burden, followed by the characteristic double-lumen pattern of SCAD, with the catheter entering into the false lumen and compression of the true lumen (figure 1C, arrow), which was causing the ring sign. Subsequently, the catheter immediately re-entered the true lumen (figure 1D), surrounded by a subintimal hamatoma (arrow). Finally, the IVUS run showed an intimal tear corresponding to the distal entry of the dissection (figure 1E, arrow), followed by normal architecture of the vessel.
The patient was managed conservatively as there were no symptoms of angina or flow limitations. Fibromuscular dysplasia was ruled out, and the patient has remained asymptomatic during follow-up.
With this case, we present a novel, undescribed «ring sign» pattern of SCAD, highlighting the crucial role of intracoronary imaging to clarify ambiguous angiographic lesions and select the most appropriate approach.
FundingNothing to declare.
ETHICAL CONSIDERATIONSThe authors attest they are in compliance with human studies and animal welfare regulations. Informed consent was obtained and the data are not identifiable. Possible sex/gender biases were considered.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence has been used in the drafting of this article.
AUTHORS’ CONTRIBUTIONSAll authors have participated, reviewed, and approved the content of this manuscript.
CONFLICTS OF INTERESTAll authors declare that there are no conflicts of interest related to this manuscript.