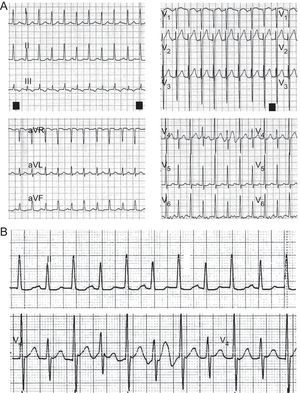
A 23-year-old man was hospitalized to undergo renal transplantation. He had a 2.5-year history of supraventricular tachycardia that was assessed in the cardiology department; structural heart disease was excluded, and the patient started beta blocker treatment. The postoperative course following kidney transplantation was favorable, but on the second day, he experienced repeated self-limited episodes of regular narrow QRS tachycardia (Figure 1A). Although the patient only perceived mild palpitations, the condition produced a situation of acute tubular necrosis due to low output. The electrocardiogram showed 2 QRS complexes for each P wave (Figure 1B) and an alternating cycle, one at 150 bpm and another at 135 bpm. Nodal nonreentrant tachycardia was suspected, based on the presence of a double nodal pathway with simultaneous anterograde conduction through both pathways in sinus rhythm. Electrophysiologic study confirmed the suspected condition by induction of repeated runs of tachycardia due to the double nodal response (Figure 2A: HRA, high right atrium; RVA, right ventricular apex; A, atrial tracing; H, His bundle; V, ventricular tracing). Ablation of the slow nodal pathway was carried out, the phenomenon disappeared, and the patient showed stable sinus rhythm (Figure 2B). On echocardiography the next day, the left ventricular ejection fraction was 41% and ventricular diameters were increased (63/54 mm). One year later, the nephrological status was favorable and the patient experienced no episodes of palpitations. Holter monitoring showed no tachycardia, sinus rhythm was stable, and the function and size of the left ventricle had completely returned to normal (ejection fraction 65%, decrease in ventricular diameters to 48/32 mm), findings that confirmed the diagnosis of tachycardiomyopathy.
ISSN: 1885-5857
Impact factor 2024
4.9