Keywords
INTRODUCTION
Arteriosclerosis is a systemic disease that can affect various vascular beds. For this reason, coexistence of coronary, peripheral, and cerebral involvement is common. Peripheral arterial disease usually occurs together with coronary disease and patients presenting this condition have a 2-fold to 4-fold higher risk of experiencing myocardial infarction and death. One-third of patients with coronary disease also have associated peripheral arterial disease.1
The internal mammary artery (IMA) is the graft of choice for coronary revascularization.2 Nevertheless, in patients with occlusive aortoiliac disease, blood flow to the lower extremities can depend to a greater or lesser extent on the collateral circulation originating in the internal mammary artery.3-5 Hence, the use of this vessel as a graft without taking the necessary precautions may result in acute ischemia of the lower limbs.6-9 We show 3 patients with Leriche syndrome and coronary disease, in whom during diagnostic procedure we performed a selective IMA angiography. This test documented collateral circulation to the ipsilateral femoral artery through abdominal anastamoses with the inferior epigastric artery.
CASE 1
A 62-year-old male ex-smoker with chronic obstructive pulmonary disease was diagnosed with Leriche syndrome in 1999. He had a single functioning kidney with right renal artery stenting through the left axillary artery since 2000. He was admitted to hospital with non-ST-segment-elevation acute coronary syndrome, with dynamic changes in the lateral derivations and elevated troponin (Tn) levels (7.7 ng/dL). His left radical and cubital arteries were filiform, and right arteries were not palpable so, coronary angiography with a 5F catheter was performed through the left brachial artery. Coronariography disclosed moderate stenosis in the middle third of the right coronary artery and proximal circumflex artery (Cx) (with contrast retention). Collateral circulation to the other vessels was observed starting from the LAD, with good distal beds.
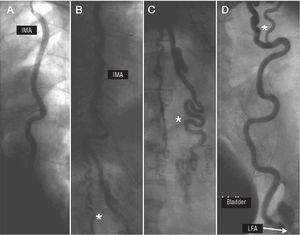
In addition, the patient had deteriorated ventricular function (ejection fraction, 40%) and moderate mitral regurgitation. Angioplasty of the culprit vessel (Cx) was attempted without success. At the end of the procedure, the left IMA was catheterized (Figure 1) and abdominal collateral circulation toward the left femoral artery was observed. Due to the vascular access, contrast injection in the right mammary was not performed. The patient remained on medical treatment and experienced slow recovery, with resolution of resting angina and symptoms of angina on exertion (functional class II).
Figure 1. A, B, C, and D are sequential images. A: catheterization of the left internal mammary artery (IMA) from the left brachial artery. B and C: anastomosis of the mammary artery to the internal iliac artery at the intra-abdominal level through collateral vessels. D: draining of the internal iliac artery in the left femoral artery (LFA).
CASE 2
A 75-year-old male ex-smoker with hypertension, dyslipidemia, and type 2 diabetes had been diagnosed in 1988 with Leriche syndrome and 3-vessel coronary disease, which was revascularized with 3 saphenous vein grafts. Currently, due to the progressive angina he was referred for coronary angiography (performed through the right radical artery with a 5F catheter). The examination showed progressive disease in the native vascular tree, patent saphenous vein grafts without significant stenosis (>50%), and good ventricular function. Abdominal aortography confirmed infrarenal occlusion, and contrast injection into the right mammary artery showed collateral circulation from this vessel to the right femoral artery. The patient improved with more intense medical treatment and is being followed up for vascular surgery (at this time he has refused any surgical intervention).
CASE 3
A 53-year-old man, current smoker of 60 cigarettes per day as the only known cardiovascular risk factor, had clinical symptoms of claudication of several yearsof evolution that had not been investigated. He was admitted to the hospital for non-ST-segment-elevation acute coronary syndrome that required mechanical ventilation for 24 hours. The electrocardiogram disclosed subepicardial ischemia in the precordial leads. Maximum levels of TnI was 4 ng/dL. The physical examination revealed absence of femoral pulses, systolic murmur in the right subclavian artery, and absence of cubital pulses in both upper limbs. Diagnostic coronary angiography was performed with a 5F catheter through a left radial access. The coronary tree showed calcification and diffuse disease with a critical stenosis in the middle segment of the LAD and good distal beds. Abdominal aortography demonstrated abdominal aorta occlusion at the infrarenal level (Figure 2, white arrows), and contrast injection in the left mammary showed collateral circulation to the deep femoral artery.
Figure 2. Occlusion of the abdominal aorta.
Because of the patient's vascular comorbidity, surgical treatment was not considered. In a second stage, the LAD was successfully treated with a percutaneous procedure by rotational atherectomy and stent implantation; the access at this time was through the left brachial artery with a 6F catheter.
DISCUSSION
Coexistence of peripheral vascular disease and coronary disease is common, since these conditions have the same risk factors.10
When deciding treatment for a patient with Leriche syndrome and coronary disease with an indication for revascularization surgery, it is important to document the origin of collateral circulation to the lower limbs. In patients with obstructive aortoiliac disease, collateral circulation may arise from the visceral or parietal branches,6 and the amount of flow from each of these vessels depends on the degree of obstruction. Therefore, the higher the aortic occlusion is, the less likely it is that collateral circulation arises from the mesenteric and lumbar arteries (and if it does, it is usually minor), and the more important is the flow from the mammary arteries.4
The IMA is the graft of choice for coronary bypass,2 particularly to the left anterior descending artery. Complications related to the use of this vessel are uncommon, but cases of acute ischemia of the lower limbs have been reported when the IMA is used in patients with occlusive aortoiliac disease.6,7,9 In these patients, the IMA can be the main source of collateral circulation to the femoral arteries and its use in myocardial revascularization has been associated with acute, sometimes severe, lower limb ischemia.6-9 Circulation from the IMA to the lower limbs occurs through anastomoses by small collaterals between the IMA and the inferior epigastric artery below the abdominal rectus muscles, and injury to these vessels during abdominal surgery (or accidental trauma) can also produce acute ischemia of the lower limbs.11,12 The percentage of flow to the lower limbs supplied by the mammary artery depends on the location of the abdominal aorta obstruction, and is greater when the obstruction is more proximal.l4
When selective angiography of the IMA is performed in these patients, it is observed that the vessel diameter is larger than normal (>3 mm), the superior and inferior epigastric arteries are more highly developed,5,13 and that intra-abdominal anastomoses are present, finally those vessels drain into the respective iliac or femoral arteries.
Our patients did not have abdominal aorta flow immediately after the origin of the renal arteries, and in all 3 patients the catheterized IMA provided blood supply to the homolateral femoral artery.
Given the consequences of this entity, it might be advisable to perform abdominal aortography in patients with a coronary condition and evidence of peripheral vascular disease, particularly those with a weak femoral pulse, intermittent claudication, or a difficult femoral access. It may be even more important to routinely perform selective angiography of the IMA in patients with aortoiliac occlusion who are potential candidates for cardiac surgery.3 Taking into account that vascular access through the upper limbs is "mandatory" (radial, brachial, and in some cases, axillary artery), catheterization of the homolateral IMA is simple.
The ideal treatment for these patients is still uncertain. Dietzek et all6 recommend avoiding use of the mammary artery for coronary revascularization and instead advocate sequential coronary-peripheral surgery. Other groups have had good results with simultaneous surgical revascularization using the mammary artery as a coronary graft and bypassing to the lower extremities, using different techniques depending on the level of the occlusion.3,14 Lastly, in some patients with considerable morbidity, angioplasty can be an equally effective alternative. Experience is limited in this area, however, and the treatment decision for each individual patient should be made by consensus among cardiologists, catheterization specialists, and cardiovascular surgeons.
Correspondence: Dr. M.C. Ferrer-Gracia.
Sección de Hemodinámica. Hospital Universitario Miguel Servet.
Paseo Isabel la Católica, 1-3. 50009 Zaragoza. España.
E-mail: mcferrergracia@yahoo.es
Received April 25, 2007.
Accepted for publication May 9, 2007