Implantation of a mechanical prosthesis in the tricuspid position is uncommon because most of the patients with disease in this valve choose to undergo repair consisting of annuloplasty. When mechanical prostheses are implanted in the tricuspid position, the risk of thrombosis is greater than that associated with these devices in left chambers, as the flow is slower in the right chambers and the pressure is lower. Currently, there is little literature on prosthetic tricuspid valve thrombosis and its treatment.
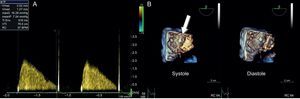
We report the case of a 52-year-old woman, with congenital atrioventricular block, who had undergone implantation of a dual-chamber pacemaker in 1986 and developed a pressure ulcer that required deepening of the pocket in 1989. Lead dysfunction occurred in 1996, and a new system was implanted, but the leads from the previous system were not withdrawn. In March 2013, she was diagnosed with severe tricuspid stenosis due to leaflet fibrosis, secondary to the leads that passed through the valve, and a 27-mm St. Jude Masters double-disc mechanical prosthesis was implanted. During the follow-up period, while asymptomatic, she reported that she no longer could hear the sounds of the prosthesis, and auscultation detected an increase in the intensity of the murmur during tricuspid filling. Doppler ultrasound revealed an increase in the atrioventricular pressure gradient across the tricuspid valve, and 3-dimensional transesophageal echocardiography demonstrated the immobility of one of the leaflets produced by a thrombus (Figure 1). At that time, she was being treated with warfarin to maintain the International Normalized Ratio (INR) between 2.5 and 3.5. Nevertheless, her medical records show suboptimal anticoagulation levels weeks before the follow-up visit (INR 2.0-2.2).
A: Doppler ultrasound at the level of the tricuspid valve prosthesis, showing an increase in the atrioventricular gradient with a decreased EF slope. B: 3-dimensional echocardiographic images at the level of the tricuspid valve prosthesis in systole and diastole, showing the immobility of one of the leaflets in systole produced by a thrombus (arrow).
The patient was admitted to the hospital and enoxaparin was added to the warfarin, at a dose of 1mg/kg body weight/12hours for 8 days. After this period, 3-dimensional transesophageal echocardiography was repeated and no changes were observed. Due to the risk of thrombus progression and its hemodynamic consequences, the decision was made to apply fibrinolysis, discontinue warfarin administration, and maintain enoxaparin. Once the INR was within normal range, 100mg of tissue plasminogen activator was infused over 3hours, with electrocardiographic monitoring and control of blood pressure and oxygen saturation; there were no complications.
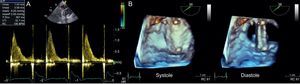
Normalization of the atrioventricular gradient was subsequently verified by Doppler ultrasound, and a 3-dimensional transesophageal echocardiogram confirmed the disappearance of the thrombus and the mobility of the 2 discs (Figure 2). At the time of discharge, she was asymptomatic.
A: normalization of the tricuspid EF slope with normalization of the atrioventricular gradient. B: 3-dimensional echocardiogram at the level of the tricuspid valve prosthesis in systole and diastole, with complete aperture and closure of the 2 discs and disappearance of the thrombus.
Currently, the little available scientific evidence regarding the most effective treatment for prosthetic tricuspid valve thrombosis is based only on case series and expert recommendations. The resolution of tricuspid valve thrombosis achieved by intensifying anticoagulation therapy or adding low-molecular-weight heparin has been reported,1 but the level of evidence is low because of the lack of randomized studies.
A recent review of 9 studies, which included 48 patients with prosthetic tricuspid valve thrombosis who received fibrinolytic therapy, demonstrated a success rate of 88%, partial success in 1 patient, and no effectiveness in 4, who underwent surgical replacement of the prosthetic valve.2
The administration of fibrinolytic therapy has been accepted as the treatment of choice for prosthetic tricuspid valve thrombosis in the latest guidelines on valve disease. It carries a IIa recommendation and level of evidence of B,3 based on nonrandomized studies and on retrospective cohort studies. No systemic embolisms were documented, although small subclinical pulmonary emboli were observed, and surgery was reserved for those cases in which fibrinolysis had been unsuccessful.
There is no specific recommendation as to which is the fibrinolytic agent of choice, and the options include streptokinase, tenecteplase, urokinase, and recombinant tissue plasminogen activator; the latter is most widely used.2,4
Transesophageal echocardiography is the technique of choice for the confirmation of both the presence of a thrombus and its resolution,5 but there are no data concerning the utility of 3-dimensional echocardiography. In the case described here, the 3-dimensional echocardiographic images clearly show both the presence and the resolution of the thrombus (video of the supplementary material).
Recurrences have been reported in nearly a third of the cases. Given the close relationship between tricuspid prosthetic valve thrombosis and suboptimal anticoagulation, it has been recommended that the INR be maintained between 3 and 4 and that acetylsalicylic acid or clopidogrel be included in the oral anticoagulation therapy.6