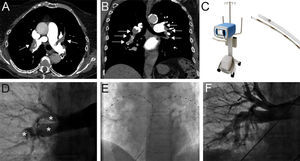
A 92-year-old woman with no medical history of note was admitted to the emergency room with sudden shortness of breath. She had tachycardia around 110 bpm, with blood pressure of 90/60mmHg and an SpO2 of 81% without oxygen support. Massive pulmonary embolism was suspected and computed tomography was immediately performed showing a bilateral submassive pulmonary embolism (Figures A and B, arrows). The performance of systemic thrombolysis was proposed, but due to the patient's advanced age and a nonnegligible risk of major bleeding, it was finally decided to perform a catheter-directed thrombolysis by using an ekosonic ultrasound-accelerated thrombolysis system (EKOS, Bothell, Washington, United States), a novel catheter-based technique that allows local low-dose thrombolysis due to an enhanced effect triggered by ultrasounds and therefore a decreased risk of major bleeding.
The EKOS system comprises 2 components: an EkoSonic control unit and a catheter with ultrasonic microtransducer core (Figure C). The baseline pulmonary angiogram showed a large amount of thrombus distributed at both the right and left main pulmonary branches (Figure D, asterisks), with poor flow toward segmental branches and poor runoff of contrast. Subsequently, the catheters were placed at both pulmonary arteries (Figure E).
A regimen of tissue-plasminogen activator (Genentech, South San Francisco, California, United States) was started at 1mg/catheter/h for 12hours, with a total dose of 24mg.
Twenty-four hours later a follow-up angiogram was performed showing almost complete resolution of the thrombus with good arborization of the segmental branches (Figure F) and no bleeding reported during hospitalization.