Percutaneous closure of paravalvular leak (PVL) has emerged as an alternative to surgery in selected patients. Several imaging modalities have been used, but predicting the number and size of devices to be implanted remains challenging. Printed 3-dimensional (3D) models have been previously shown to be useful for some structural interventions. Nevertheless, to the best of our knowledge, there have been no descriptions of their feasibility in PVL closure preprocedural planning. We present these two 3D-printing PVL cases as feasibility/proof-of-concept.
Based on cardiac-computed tomography data, segmentation was performed using free-software ITK-SNAP. The models were fabricated in polyurethane filament by fused deposition modelling. An experienced operator used this model to select the number and size of devices to be deployed during the procedure.
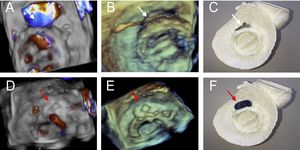
The first case was a 78-year-old man admitted for heart failure due to severe PVL over a mitral mechanical prosthetic valve (Figure 1). The defect was anterolateral (white arrow), 11.9 × 3.6mm on 3D-transesophageal echocardiography (TEE) (12.2 × 3.5mm on 3D-printing). After closure (AVP [Amplatzer Vascular Plug]-III 12 × 5mm, red arrow), no significant regurgitation was observed on color 3D-TEE.
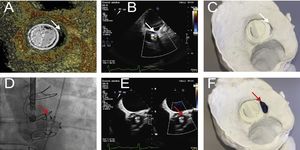
The second case was an 81-year-old man also admitted for heart failure due to PVL over an aortic mechanical prosthetic valve (Figure 2). Computed tomography and TEE showed a 13.8 × 4mm semilunar shape PVL (white arrow) on the left aortic sinus. The 3D-printed model (view from ventricular aspect) revealed left PVL with the same measures. After catheter-based closure (AVP-III 14 × 5mm, red arrow), no significant residual regurgitation was detected.
CONFLICTS OF INTERESTI. Cruz-González is proctor for Abbot.