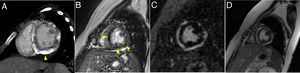
A 12-year-old girl presented with fever, dyspnea, and lower limb edema for 7 days. Blood tests depicted high C-reactive protein, d-dimer and troponin levels, and urinalysis showed hematuria and proteinuria. An echocardiogram identified severe systolic dysfunction (left ventricular ejection fraction of 28%) and head computed tomography (CT) depicted chronic sphenoidal sinusitis. Chest CT identified pulmonary cavities and nodules with halo sign, suggestive of vasculitis, and diffuse subepicardial enhancement in the left ventricle, suggestive of myocarditis (figure 1), and no ventricular calcifications. Subsequent investigation revealed antineutrophil cytoplasmic antibody positivity. The patient fulfilled 4 of the 6 criteria of the 2008 European League Against Rheumatism/Paediatric Rheumatology European Society (EULAR/PRES) for childhood granulomatosis with polyangiitis (GPA). At least 3 criteria are necessary to confirm the diagnosis. During the acute phase, the patient was in no condition to undergo cardiac magnetic resonance. Follow-up examinations after 4 months of immunosuppressive therapy depicted moderate systolic dysfunction (left ventricular ejection fraction of 34%), pericardial effusion (asterisk in figure 2) and diffuse dystrophic left ventricular calcifications (arrowhead in figure 2). After 5 months of follow-up, there was an improvement in the pericardial effusion, persistence of subepicardial left ventricular calcifications (more easily depicted in the CT - arrowheads in figure 3A,B) and identification of early (figure 3C) and late (figure 3D) subepicardial left ventricular gadolinium enhancement. We obtained written informed consent from our patient's guardian for the publication of this case.
GPA is uncommon in children and cardiac manifestations are rare. The most frequent cardiac manifestations are pericarditis, cardiomyopathy, and coronary artery disease. To the best of our knowledge, this is the first reported case of acute myocarditis in juvenile-onset GPA.
FUNDINGThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
AUTHORS’ CONTRIBUTIONSA. Vaz conceived the analysis, and wrote and reviewed the paper. C. Pietroski Reifegerste collected the data and reviewed the paper. B. Maurício Pedrazzani guided the preparation of the work and reviewed the paper.
CONFLICTS OF INTERESTThe authors declare that they have no competing interests.