A 10-year-old boy with no past medical history was investigated in our department for chest pain on exertion. On physical examination, a grade 2/6 systolic murmur at the left upper sternal border radiating to the interscapular area was identified. Blood pressure in the right and left arms were 160/95 mmHg and 100/75 mmHg, respectively. Femoral and left brachial pulses were palpable bilaterally but weak and delayed compared with the right brachial pulse. Electrocardiogram revealed left ventricular hypertrophy and T-wave inversion in inferolateral leads. This article received was approved by the Ethics committee of our center. Written informed consent from the patient's parents was obtained.
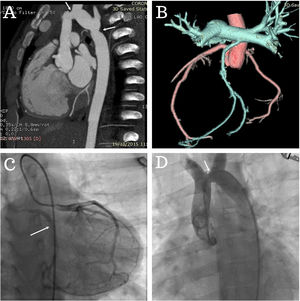
Echocardiography findings were left ventricle hypertrophy with normal wall motion and systolic ejection fraction, a nonstenotic bicuspid aortic valve and an atypical coarctation of the aorta just proximal to the left common carotid artery. Computed tomography angiography revealed severe aorta coarctation with double constriction proximal to the origin of the left common carotid artery and distal to the left subclavian artery (figure 1A, arrows) with an anomalous origin of the circumflex coronary artery from the right pulmonary artery (figure 1B).
The patient underwent cardiac catheterization to evaluate his coronary artery disease and the severity of the coarctation. Left coronary angiography showed a retrograde filling of the circumflex coronary artery from the left anterior descending artery which arises from the pulmonary artery (figure 1C, arrow; ).
Aortography revealed the unusual site of coarctation (figure 1D, arrow; ). In the hemodynamic study, peak-to-peak gradients from both locations were 30mmHg (ascending aorta to distal aortic arch) and 15mmHg (pre- and postsubclavian artery), respectively. After multidisciplinary consultation within the Heart Team, a staged approach was planned with balloon angioplasty of the proximal site of the coarctation first, followed by ischemia-guided surgical repair of the anomalous origin of the circumflex coronary artery.
FUNDINGNo fund was received.
AUTHORS’ CONTRIBUTIONSM. Slim collected data, figures and videos. R. Gribaa drafted the manuscript. All authors discussed the results and contributed to the final manuscript.
CONFLICTS OF INTERESTNothing to disclose.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2021.03.001