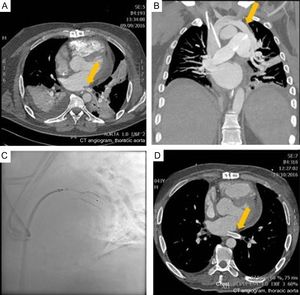
A 42-year-old man was seen for slowly progressive dyspnea (New York Heart Association functional class III/IV). He had had a history of atrial fibrillation since he was 26 years old, and had undergone several pulmonary vein ablations, the most recent of which was a surgical procedure (maze IV biatrial procedure) 1 year previously. An echocardiogram showed severe posterior pericardial effusion affecting the left ventricle; the right ventricle was moderately dilated, hypertrophic, and mildly dysfunctional. Surgical drainage was performed by anterior minithoracotomy given the poor accessibility, and the procedure produced 400mL of hematic fluid. The patient́s condition worsened, with the appearance of respiratory distress. On chest computed tomography (CT), severe stenosis was observed in the left inferior pulmonary vein, proximal to the left ventricular outlet (Figure A, arrow), as well as anomalous venous drainage to the left superior pulmonary vein in the innominate vein-right atrium (Figure B, arrow), leading to a left-right shunt. Angioplasty was performed, with placement of 2 stents (Figure C), overlapping in the stenotic region of the left inferior pulmonary vein. The procedure was successful. Follow up CT showed a decrease in the extent of anomalous venous drainage and a patent pulmonary vein stent (Figure D, arrow).
Partial anomalous venous drainage is considered a minor cardiac disease due to the small volume of the shunt, with little clinical repercussion. It is therefore underdiagnosed. With sufficient clinical suspicion, it can be diagnosed by echocardiography. In the case of a poor echocardiographic window, CT can be used. This enables screening for structural heart disease in young patients with atrial fibrillation. This is essential before proceeding to ablation.