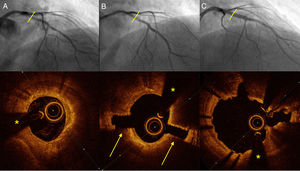
A 71-year-old male exsmoker with hypertension, diabetes and dyslipidemia was admitted for unstable angina. Angiography showed a severe long and calcified lesion from the left main coronary artery to the proximal and medial left anterior descending (LAD) artery. Figure 1 () shows the optical coherence tomography (OCT) image acquired before coronary lithotripsy (CL). Severe circumferential calcification was observed in the proximal LAD lesion (* guidewire artefact), with an OCT-calcium score of 4. This score is a predictor of inadequate expansion (maximum calcium thickness> 0.5mm,> 180°, length>5mm). Angioplasty was performed by CL (shockwave intravascular lithotripsy) with a 3×12mm balloon at 4atm for 10seconds, applying 2 pulses to the medial LAD artery and 1 to the proximal LAD artery (balloon rupture occurred on opening of the proximal lesions at 6 atm; nominal diameter/vessel ratio=0.9). Figure 1B () shows the outcome immediately after CL at the same point of the proximal LAD. Complete fractures of the circumferential calcium with a depth of up to 1.4mm (arrows) can be seen. These had no impact on the adventitia of the vessel. Plaque preparation was completed by predilatation with a cutting balloon (3×10mm) and, under OCT imaging guidance, 2 overlapping drug-eluting stents were implanted. Figure 1C () shows the follow-up OCT image after stent placement. Displacement of the fractures can be seen with acute luminal gain, enabling appropriate stent expansion and minimal residual malapposition.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2014.04.021