At present, balloon angioplasty of the pulmonary arteries is an effective therapeutic option in chronic thromboembolic pulmonary hypertension. The use of the pressure wire increases the safety of these procedures as it reduces the extent of reperfusion edema. Moreover, it allows a similar hemodynamic improvement with fewer treated lesions and fewer angioplasty sessions.
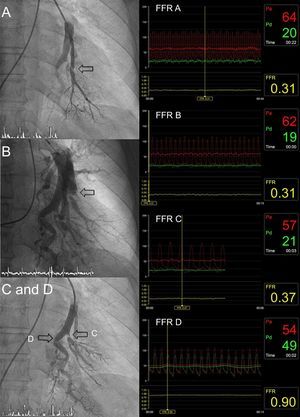
We discuss the usefulness of the pressure wire for identifying those lesions that are amenable to angioplasty in a patient with inoperable chronic thromboembolic pulmonary hypertension. The first pulmonary angioplasty procedure focused on the segmental branches of the left lower lobe, using the pressure wire as a guidewire for angioplasty. We analyzed the fractional flow reserve (FFR) distal to the lesions to be treated and performed angioplasty when the FFR was < 0.80. In 3 segmental branches, functional assessment revealed a FFR < 0.80 and a highly damped pressure curve, similar to the pulmonary wedge pressure; these branches were treated (Figures A, B, and C, arrows). However, in a fourth segmental branch that we had planned to treat, the angiographic image of the membrane did not correlate with the functional level. We found a FFR = 0.90 and a morphologically normal pressure curve (Figure D, arrow), and ruled out the need to treat this lesion.
Thus, the pressure wire avoids unnecessary interventions in branches that are not affected by the distal flow. This allows interventions to focus on those lesions that will show a clinical benefit from treatment, thus reducing the risks and increasing the efficacy of the procedures.