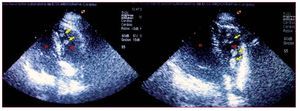
A 58-year-old woman with dilated myocardial disease of ischemic origin had received a heart transplant 2 months earlier, with no postoperative complications. She was discharged from the hospital and came for her sixth heart biopsy, which could not be performed because of occlusion of both jugular accesses (Figure 1). Transthoracic echocardiography was performed to rule out a possible rejection. The apical 4-chamber view (Figure 2) showed a mobile vegetative mass in the right atrium that protruded toward the right ventricle (RV) through the tricuspid valve, and another mass in the apex of the RV. Both features were consistent with fresh thrombi. The patient was hospitalized, and because of the absence of contraindications, thrombolysis was started (100 mg intravenous alteplase). On ultrasound follow-up 24 h after the treatment, both thrombi of the right chambers were seen to have disappeared with no embolic or hemorrhagic complications.
Figure 1.
Figure 2.
In an attempt to clarify the possible causes of the thrombophilia, a hypercoagulability study was performed, in which the main anomalies related with venous thrombosis were analyzed; however, the results were normal. The patient's medical history showed that before transplantation she had been under treatment with acenocoumarol for chronic atrial fibrillation; the treatment had been initiated 8 years earlier because of an episode of deep vein thrombosis following immobilization due to trauma. Ultimately, she was treated with low molecular weight heparin (enoxaparin 60 mg/12 h) until anticoagulation was achieved with acenocoumarol.
This is a rare case of venous and right-chamber thrombosis in a heart transplant recipient that resolved successfully, and for which no apparent cause could be identified.