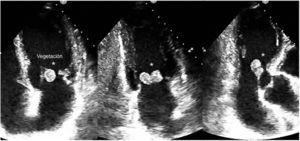
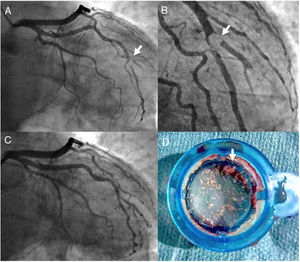
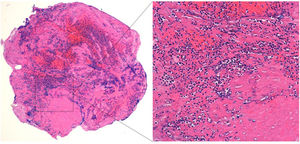
A 62-year-old man with no relevant medical history was admitted to hospital after reporting fever and weight loss during the preceding month. Blood cultures revealed methicillin-resistant Staphylococcus aureus bacteremia, and abdominal computed tomography detected evidence of splenic infarctions. Transthoracic echocardiography () revealed endocarditis in the native mitral valve, with vegetations on the atrial surface of both leaflets. The larger vegetation (10×25mm) was attached to the anterior leaflet (Figure 1, asterisk) and was causing moderate regurgitation. During the fourth day of hospitalization, the patient complained of severe chest pain at rest. The electrocardiogram showed a 2mm ST-segment elevation in the inferior and lateral leads. Emergency coronary angiography () detected a subocclusive lesion of embolic appearance in the first bifurcated marginal branch (Figure 2A and B, arrow). Intracoronary aspiration thrombectomy allowed repurfusion of the occluded artery (Figure 2D), and there was no evidence of atherosclerotic lesions (). Pathological analysis of the aspirated material (Figure 2D, arrow) revealed a myxoid tissue with abundant polymorphonucleocyte infiltration (Figure 3), and microbiology confirmed S. aureus infection. The patient underwent emergency surgery to replace the mitral valve with a mechanical prosthesis and recovered without incident.
Acute myocardial infarction is an infrequent complication in patients with infective endocarditis; differential diagnosis includes extrinsic coronary compression and an embolism of infective material. In this case, aspiration thrombectomy allowed reperfusion of the vessel and confirmation of the diagnosis of myocardial infarction secondary to septic embolism.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2019.04.007.