Penetrating wounds of the heart are extreme medical emergencies. Only 11% to 20% of patients are hemodynamically stable on reaching hospital and can benefit from surgical treatment. The right ventricle (RV) is the heart chamber most commonly implicated in cardiac tamponade when bleeding occurs in the pericardial sac, and hypovolemic shock when the wound communicates with the thorax.
We present the case of a 17-year-old adolescent boy with a knife wound in the left fifth intercostal space. On hospital arrival, his vital signs were stable and the cardiopulmonary auscultation was normal. Electrocardiography showed a generalized concave ST-segment elevation in all leads. Laboratory analyses yielded normal results.
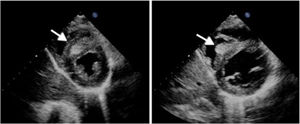
The echocardiogram showed a mild pericardial effusion. The interventricular septum (IVS) was thickened, and there was a mass of intermediate echogenicity with scalloped borders protruding towards the RV, suggestive of a traumatic thrombus/hematoma due to puncture of the ventricle apex (Figure 1 and ).
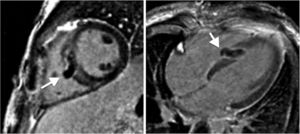
Evaluation with contrast-enhanced cardiac magnetic resonance imaging depicted an avascular area in the middle IVS, consistent with the thrombotic material protruding into the RV chamber (Figure 2). As the patient was clinically and hemodynamically stable, an expectant attitude was adopted, with analgesia and close monitoring by echocardiography.
At 15 days, echocardiography showed a significant reduction in IVS thickness and resolution of the pericardial effusion ().
On follow-up cardiac magnetic resonance imaging, the thrombus had resolved and there was a residual scar in the IVS. The patient remained asymptomatic over follow-up (Figure 3).
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2019.03.017.